kottke.org posts about medicine
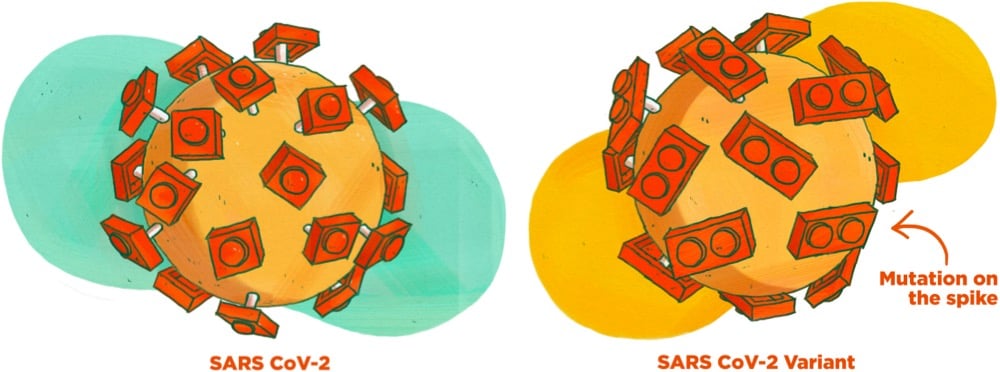
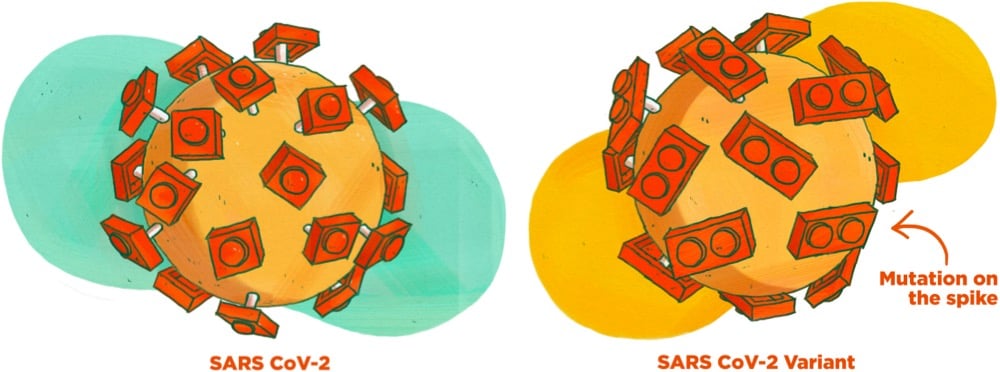
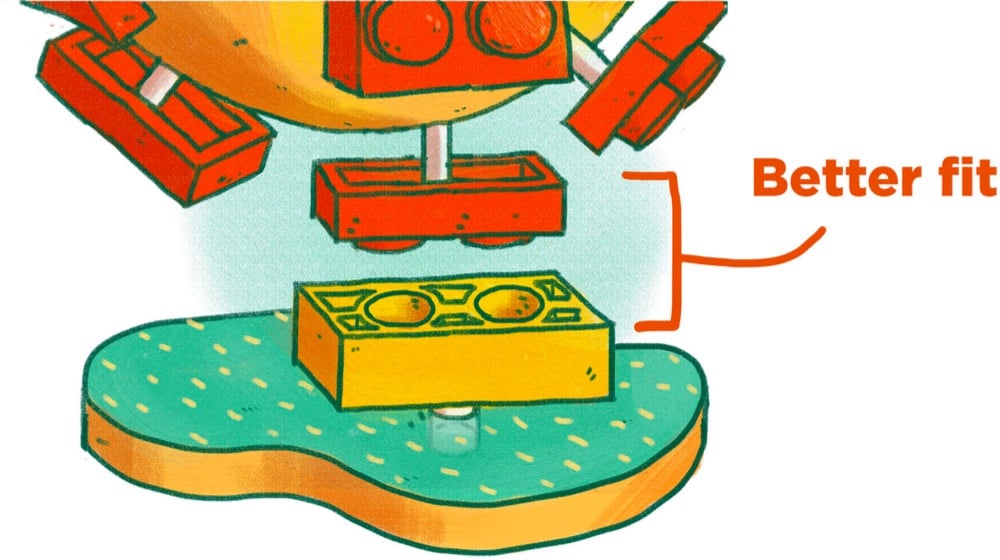
This guide to Covid-19 variants (SARS-CoV-2 viruses that have evolved changes to meaningfully alter their behavior) by Michaeleen Doucleff and Meredith Rizzo at NPR cleverly visualizes how mutations of the virus’s spike proteins help bind it more easily to ACE2 receptors on human cells. The key to the visualization is Meredith Miotke’s illustrations of the viruses using Lego pieces to represent the virus spikes and cell receptors. The usual SARS-CoV-2 has 1x1 Lego pieces that can bind with 1x2 pieces, like so:
But, as everyone who has ever worked with a Lego set knows, a 1x1 piece stuck to a 1x2 piece is not super stable. So when a version of the virus with a 1x2 piece shows up, it’s able to form a better connection to the 1x2 receptor:
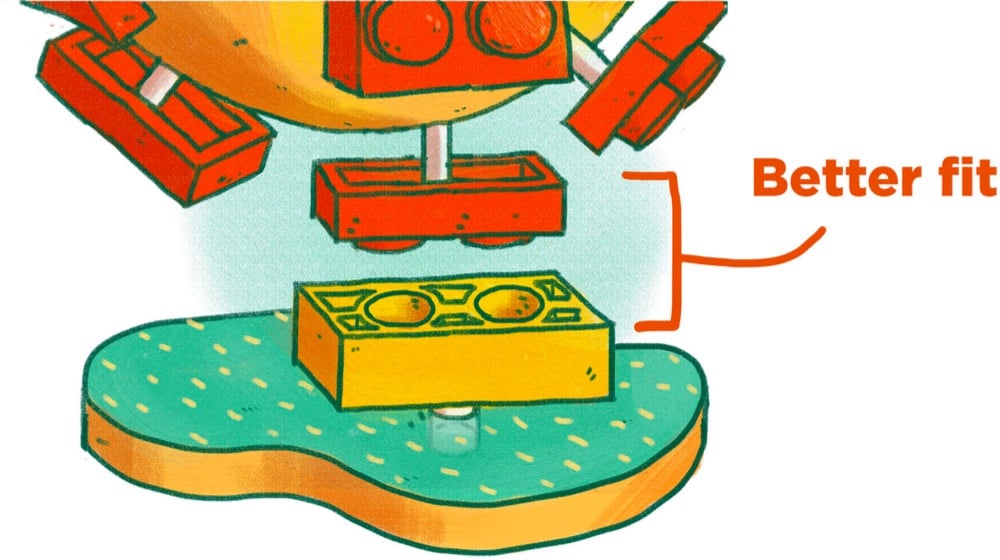
The analogy breaks down if you look too hard at it1 but for many people, it can be a quick way to get the gist of the mechanism at work here. (via @EricTopol)

You probably read something yesterday, maybe just a headline, about Moderna’s Covid-19 vaccine being “six times less effective” against the B.1.351 coronavirus variant first identified in South Africa. This is, to put it plainly, a bullshit take on what is actually excellent news. This is the important bit, via Stat:
Both the Moderna vaccine and the immunization from Pfizer-BioNTech produce such powerful levels of immune protection — generating higher levels of antibodies on average than people who recover from a Covid-19 infection have — that they should be able to withstand some drop in their potency without really losing their ability to guard people from getting sick.
“There is a very slight, modest diminution in the efficacy of a vaccine against it, but there’s enough cushion with the vaccines that we have that we still consider them to be effective,” Anthony Fauci, the top U.S. infectious diseases official, said Monday on the “Today” show.
Let’s hear that again: “Both the Moderna vaccine and the immunization from Pfizer-BioNTech produce such powerful levels of immune protection…” These vaccines are so good, so potent, that even this sixfold drop in one measure of the vaccines’ ability to neutralize this one SARS-CoV-2 variant isn’t even enough to significantly reduce their overall protective power.1 That’s the important news here, that’s the very good news, that’s what you should be taking away from this. We have miraculously developed a near-perfect medicine for a plague that has significantly disrupted all human life on Earth and we’re flipping out over some technical details that the experts assure us don’t mean much in terms of overall effectiveness?! No thank you. Not today.
In a Twitter thread, Zeynep Tufekci is tearing her hair out because of the media’s misunderstanding and sensationalization of the “sixfold drop”.
I know people are tired but needless anxiety isn’t helping us. Let’s focus on getting through these months — better masks if indoors with others, more strict attention to our precautions — and the real problem: making more of these amazing vaccines quickly & getting them out there!
I get it, we want to understand but not how it works. Stop worrying about Nab titers. That does NOT mean the vaccine is six times less effective. People whose job it is to worry about it are on it & we just got confirmation: it works against the variants.
Plea to media: this isn’t a good headline. It makes people think the vaccine is six times less effective against the new variants (FALSE!) when the news today is *excellent*: The vaccine continues to work well against the new variants. That’s the headline.
For a much more technical take on the efficacy of the vaccines against variants, see virologist Florian Krammer’s long thread. His conclusion:
mRNA vaccines induce very high neutralizing antibodies after the second shot (consistently in the upper 25-30% of what we see with convalescent sera). If that activity is reduced by 10-fold, it is still decent neutralizing activity that will very likely protect. Furthermore, we know that the mRNA vaccines are already protective after the first shot when neutralizing antibody titers are low or undetectable in most individuals.
There is a concern here and it’s that B.1.351 or B.1.1.7 might mutate into variants that are significantly resistant against the vaccines’ good effects. Krammer again:
First, we need to do what every good scientist is praying for a year now: We need to cut down on virus circulation. The more the virus replicates, the more infections there are the higher are the chances for new variants to arise. Also, we need to try and contain B.1.351 and B.1.1.248/P.1 as much as possible.
That’s why, aside from preventing hundreds of thousands of deaths in the next several months, getting these vaccines into people’s arms is so important: the less the virus spreads, the less opportunity it will have to mutate into something even more dangerous. The US vaccination effort is slowly ramping up — we’re at an average of 1.3 million doses per day right now and the trend is heading in the right direction. We can get this done!
So what can you do about this right now? 1. Stop worrying about the variants until the experts let us know we have something to worry about. 2. If you are eligible for the vaccine, get it! 3. Spread the word about vaccine availability in your area. Yesterday Vermont opened signups for vaccination appointments for all Vermonters 75 and older, and I texted/emailed everyone I could think of who was over 75 or who had parents/relatives/friends who are over 75 to urge them to sign up or spread the word. 4. Continue to wear a mask (a better one if possible), wash your hands, social distance, stay home when possible, don’t spend time indoors w/ strangers, etc. Thanks to these remarkable vaccines, real relief is in sight — let’s keep on track and see this thing through.
In response to comments about a video of him getting the Covid-19 vaccine — “Come with me if you want to live!” — Arnold Schwarzenegger says that if you want to build biceps, you should listen to him. He’s the expert. But if you want to know what to do about Covid-19, you should listen to epidemiologists and doctors.
Dr. Fauci and all of the virologists and epidemiologists and doctors have studied diseases and vaccines for their entire lives, so I listen to them and I urge you to do the same. None of us are going to learn more than them by watching a few hours of videos. It’s simple: if your house is on fire, you don’t go on YouTube, you call the damn fire department. If you have a heart attack, you don’t check your Facebook group, you call an ambulance. If 9 doctors tell you you have cancer and need to treat it or you will die, and 1 doctor says the cancer will disappear, you should always side with the 9. In this case, virtually all of the real experts around the world are telling us the vaccine is safe and some people on Facebook are saying it isn’t.
In general, I think if the circle of people you trust gets smaller and smaller and you find yourself more and more isolated, it should be a warning sign that you’re going down a rabbit hole of misinformation. Some people say it is weak to listen to experts. That’s bogus. It takes strength to admit you don’t know everything. Weakness is thinking you don’t need expert advice and only listening to sources that confirm what you want to believe.
In an opinion piece for the NY Times, Zeynep Tufekci and epidemiologist Michael Mina are urging for new trials of the Moderna and Pfizer/BioNTech Covid-19 vaccines to begin immediately to see how effective a single dose might be in preventing new infections. If the trials do indicate that a single dose works, that would effectively double the number of people we could vaccinate within a certain time period, saving countless lives in the US and worldwide.
Both vaccines are supposed to be administered in two doses, a prime and a booster, 21 days apart for Pfizer and 28 days for Moderna. However, in data provided to the F.D.A., there are clues for a tantalizing possibility: that even a single dose may provide significant levels of protection against the disease.
If that’s shown to be the case, this would be a game changer, allowing us to vaccinate up to twice the number of people and greatly alleviating the suffering not just in the United States, but also in countries where vaccine shortages may take years to resolve.
But to get there — to test this possibility — we must act fast and must quickly acquire more data.
For both vaccines, the sharp drop in disease in the vaccinated group started about 10 to 14 days after the first dose, before receiving the second. Moderna reported the initial dose to be 92.1 percent efficacious in preventing Covid-19 starting two weeks after the initial shot, when the immune system effects from the vaccine kick in, before the second injection on the 28th day
That raises the question of whether we should already be administrating only a single dose. But while the data is suggestive, it is also limited; important questions remain, and approval would require high standards and more trials.
The piece concludes: “The possibility of adding hundreds of millions to those who can be vaccinated immediately in the coming year is not something to be dismissed.”
The NY Times recently surveyed 700 epidemiologists about how they are personally living during the pandemic and what they think is going to happen next. Epidemiologists should have a better idea than most of us about how to act during a viral pandemic, so there’s lots of good information in there about vaccines and high-risk behaviors. But I found their answers to a pair of speculative questions about a return to normalcy most interesting.
How and when will life go back to normal?
“For some, it has gone back to normal, and because of this, it will be two to three years before things are back to normal for the cautious, at least in the U.S.”
- Cathryn Bock, associate professor, Wayne State University
“The new normal will be continued masking for the next 12 to 18 months and possibly the next few years. This is a paradigm shift.”
- Roberta Bruhn, co-director, Vitalant Research Institute
What will never return to normal?
“My relationships with people who have taken this pandemic lightly and ignored public health messages and recommendations.”
- Victoria Holt, professor emeritus, University of Washington
“Every part of my daily life that involves interaction with anyone other than my spouse.”
- Charles Poole, associate professor, University of North Carolina
For many people, the pandemic has altered almost every aspect of their lives. If we listen to what epidemiologists are telling us (like we should have back in early 2020 to avoid much of our present hardship), it could help us accept that the pandemic will continue to affect most aspects of our lives even after it is “over”.
Free Covid-19 illustration courtesy of Pixel True.
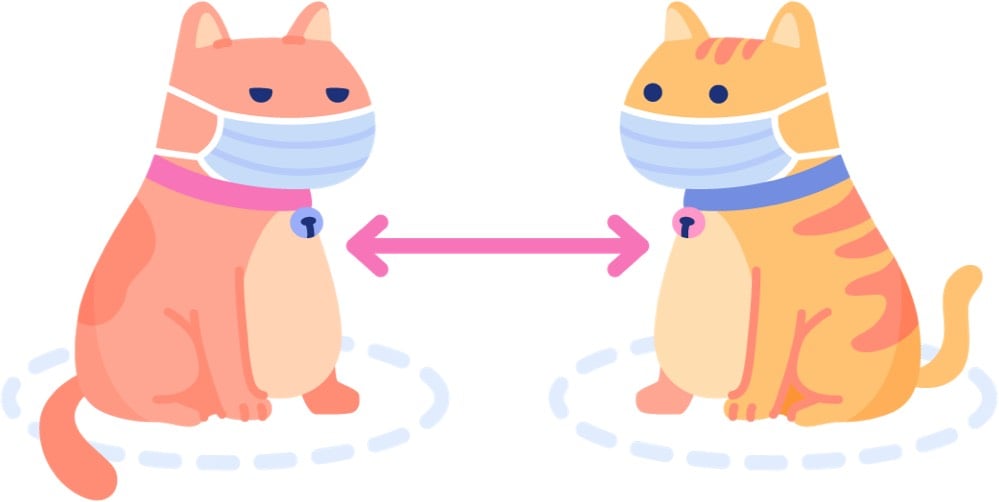
Zeynep Tufekci reports on a small study from Korea that has big implications on how we think about transmission of SARS-CoV-2. Scientists traced two cases back to a restaurant and discovered that transmission had occurred over quite a long distance in a very short period of time.
If you just want the results: one person (Case B) infected two other people (case A and C) from a distance away of 6.5 meters (~21 feet) and 4.8m (~15 feet). Case B and case A overlapped for just five minutes at quite a distance away. These people were well beyond the current 6 feet / 2 meter guidelines of CDC and much further than the current 3 feet / one meter distance advocated by the WHO. And they still transmitted the virus.
As Tufekci goes on to explain, the way they figured this out was quite clever: they contact traced, used CCTV footage from the restaurant, recreated the airflow in the space, and verified the transmission chain with genome sequencing. Here’s a seating diagram that shows the airflow in relation to where everyone was sitting:
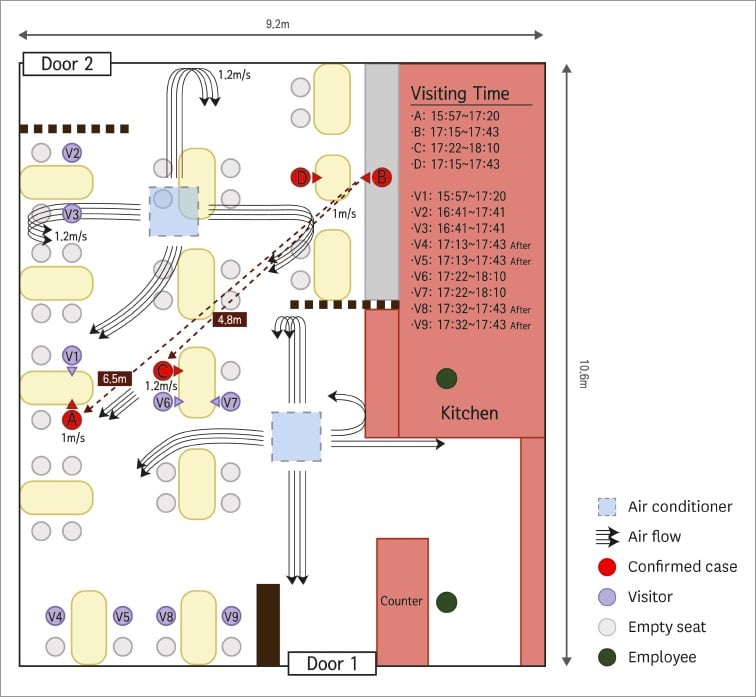
Someone infecting another person 21 feet away in only five minutes while others who were closer for longer went uninfected is an extraordinary claim and they absolutely nailed it down. As Sherlock Holmes said: “Once you eliminate the impossible, whatever remains, no matter how improbable, must be the truth.” And the truth is that in some cases, the recommended 6 feet of distance indoors is not sufficient when people aren’t wearing masks. Airflow matters. Ventilation matters. Which way people are facing matters. How much people are talking/laughing/yelling/singing matters. Masks matter. 6 feet of distance does not confer magical protection. All that can make it tough to figure out if certain situations are safe or not, but for me it’s an easy calculation: absolutely no time indoors with other people not wearing masks. Period. As Tufekci concludes:
I think there are three broad lessons here. One, small data can be extremely illuminating. Two, air flow and talking seem to matter a great deal. Three, sadly, indoor dining and any activity where people are either singing or huffing and puffing (like a gym) indoors, especially with poor ventilation, clearly remains high risk.
Read her whole post — as she says, it’s “perhaps one of the finest examples of shoe-leather epidemiology I’ve seen since the beginning of the pandemic”.
With the first approved Covid-19 vaccines set to roll out in the US soon, some of the focus has shifted to how the vaccine will be distributed and its equitable allocation. Part of the distribution logistics puzzle is making sure there are enough glass vials to hold and transport the vaccine around the nation to those waiting to be vaccinated. For the New Yorker, Christopher Payne took some photos of two Corning factories that are manufacturing vials as fast as they can.
But back in the early 19th century, for a colonial empire dealing with overseas smallpox epidemics, glass vials were not an option. Smallpox vaccination at that time was most reliably accomplished by transferring material from cowpox blisters on one person (or cow) to another person. The freshly inoculated person got a little sick but later proved to be immune to the much deadlier smallpox. So when Spain’s Royal Philanthropic Vaccine Expedition set sail in 1803 to inoculate the inhabitants of their overseas colonies for smallpox, they used the bodies of human beings to transport the vaccine. To be more specific, they used “twenty-two orphan boys, ages three to nine”.1
And so it was that, “in the era before refrigeration, freeze-dried vaccines, and jet aircraft,” writes medical historian John Bowers, “the successful circumnavigation of the globe with the vaccine…rested on a single medium — little boys.” During the long crossing, approximately twenty-two orphans who had not previously contracted smallpox or cowpox were “vaccinated in pairs every ninth or tenth day,” via arm-to-arm inoculation (taking lymph from an unbroken pustule on a recently vaccinated boy and introducing it under the skin of another). This created a vaccine chain — the vaccine remained active and viable for the entire journey.
The three-year expedition was success and an early & effective example of philanthropic healthcare, but you also have to note here that the reason the Americas were ravaged by smallpox was because Spain brought it there in the first place.
Update: In The Atlantic, Sam Kean provides some more detail on the vaccination effort.
Given the era, it’s likely that no one asked the orphans whether they wanted to participate — and some seemed too young to consent anyway. They’d been abandoned by their parents, were living in institutions, and had no power to resist. But the Spanish king, Carlos IV, decided to make them a few promises: They would be stuffed with food on the voyage over to make sure they looked hearty and hale upon arrival. After all, no one would want lymph from the arm of a sickly child. Appearance mattered. And they’d get a free education in the colonies, plus the chance at a new life there with an adoptive family. It was a far better shake than they’d get in Spain.
In an incredible effort, science has provided the world with what looks like an incredibly effective vaccine for Covid-19. For Stat, Helen Braswell writes about the challenges of turning that vaccine into vaccinations. In the US, despite heroic work from individuals and individual groups, our public health system has proved unequal to the challenge of addressing the pandemic, and we’re now turning, in part, to that system to distribute and administer the vaccines, as well as to educate the public and drum up support for vaccination. The people that we’re counting on are public officials and healthcare workers worn out from what is essentially one 9-month-long wave of illness, hospitalizations, and death across the country. Misinformation and skepticism of science and government has sowed “justified distrust” about vaccines in many people:
Concern about the vaccines, however, cuts across ethnic and socioeconomic groups. President Trump’s overt efforts to pressure the FDA to issue EUAs before the Nov. 3 election — before the vaccine trials were finished — has deepened the sense of unease. The CDC’s early pandemic testing fiasco, coupled with its sidelining by the Trump administration, has eroded its standing as a trusted source of information.
Alison Buttenheim, an associate professor of nursing and health policy at the University of Pennsylvania, refers to the current situation as a perfect storm of “justified distrust.”
“People who don’t think twice about vaccinating their kids totally on time, who get their flu shot every year, are in the sort of, ‘Hmmm. Might wait six months on this one,’” Buttenheim, who works on vaccine acceptance, told STAT. “I’ve heard people say, ‘I’ll get the European one,’” she said, adding other people have said they would get vaccinated after Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, gets vaccinated.
And it’s not just the general public. A recent survey of 2,000 doctors and nurses in New Jersey found that 60% of doctors planned to take a Covid vaccine, but only 40% of nurses intended to, Health Commissioner Judith Persichilli said in a recent “60 Minutes” segment about Operation Warp Speed.
Fauci, along with other respected public health officials and workers, should get vaccinated live on CNN. Stream it on YouTube and Twitch. It won’t convert the anti-vax, anti-mask, QAnon wingnuts (nothing will) but if you can at least get healthcare workers and at-risk folks on board, it would be time well spent.
But that’s only one small piece of the puzzle. Braswell’s piece is long and comprehensive look at the challenges regarding the Covid-19 vaccines and is worth reading all the way through.
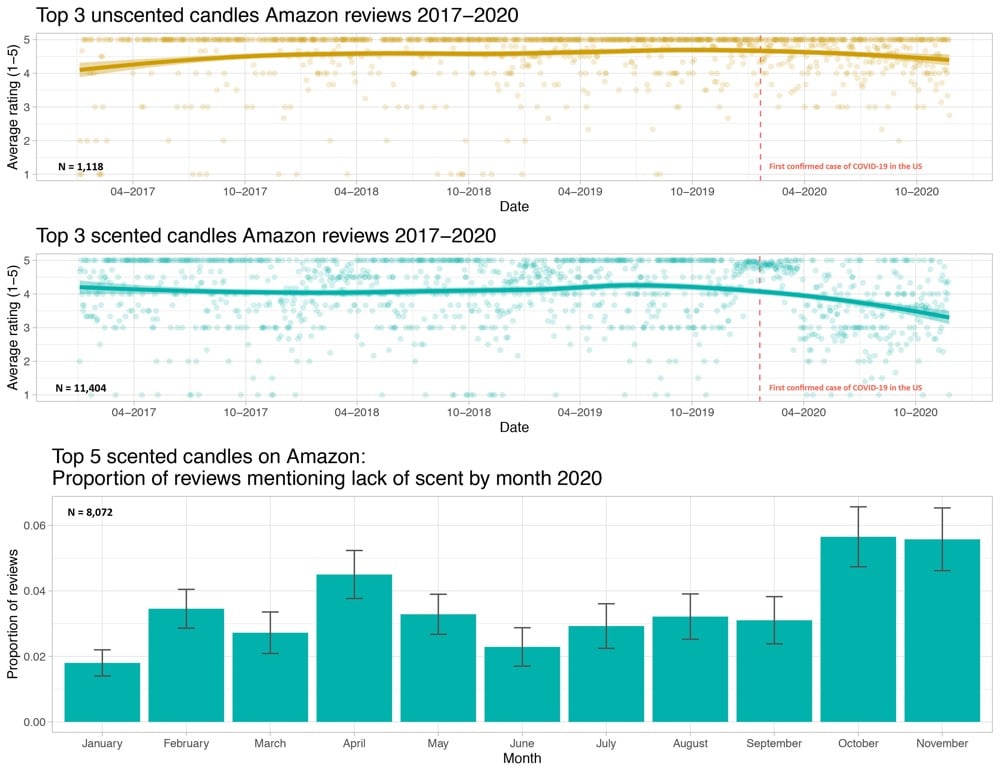
After Terri Nelson noticed people complaining online about a lack of scent from newly purchased scented candles, Kate Petrova analyzed Amazon reviews for candles from the past three years and found a drop in ratings for scented candles beginning in January 2020 (compared to a smaller ratings decline for unscented candles).
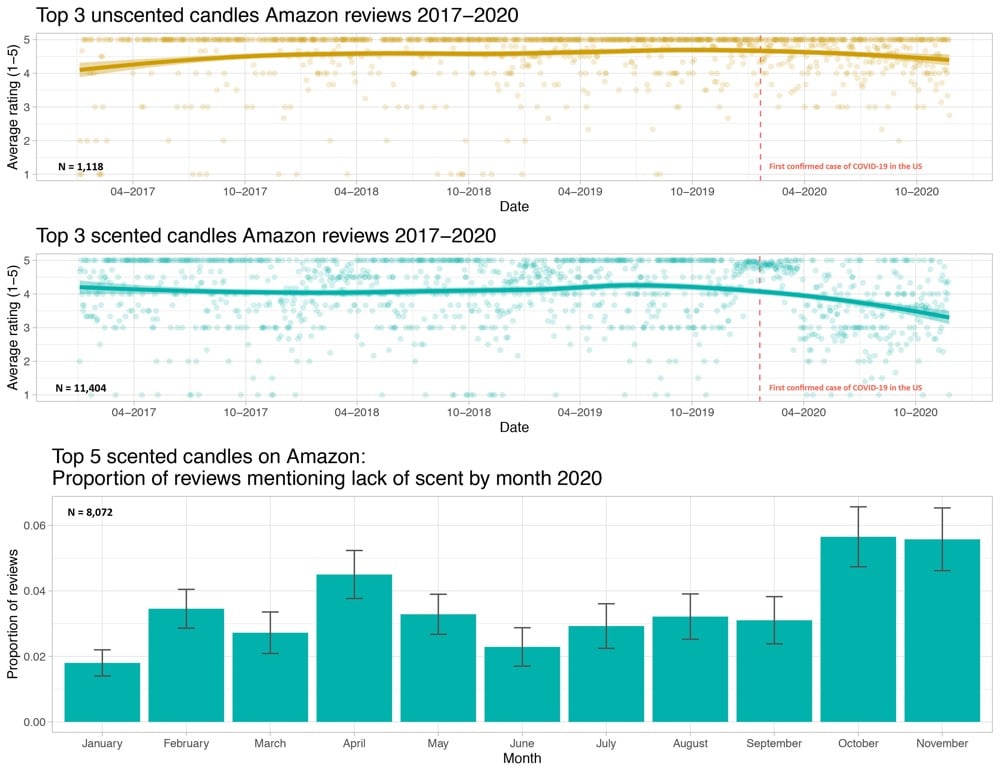
The hypothesis is that some of these buyers have lost their sense of smell due to Covid-19 infections and that’s showing up in the ratings.
Now that the preliminary results of various Covid-19 vaccine trials are coming out (and looking promising), attention is turning to the eventual distribution of the vaccines. The logistics of getting the doses out to hospitals, clinics, and doctor’s offices is one concern but so is the question of who should get vaccinated first. Supplies of the vaccines will be limited at first, so we’ll need to decide as a society what distribution method is most fair and is of the most benefit to the greatest number of people.
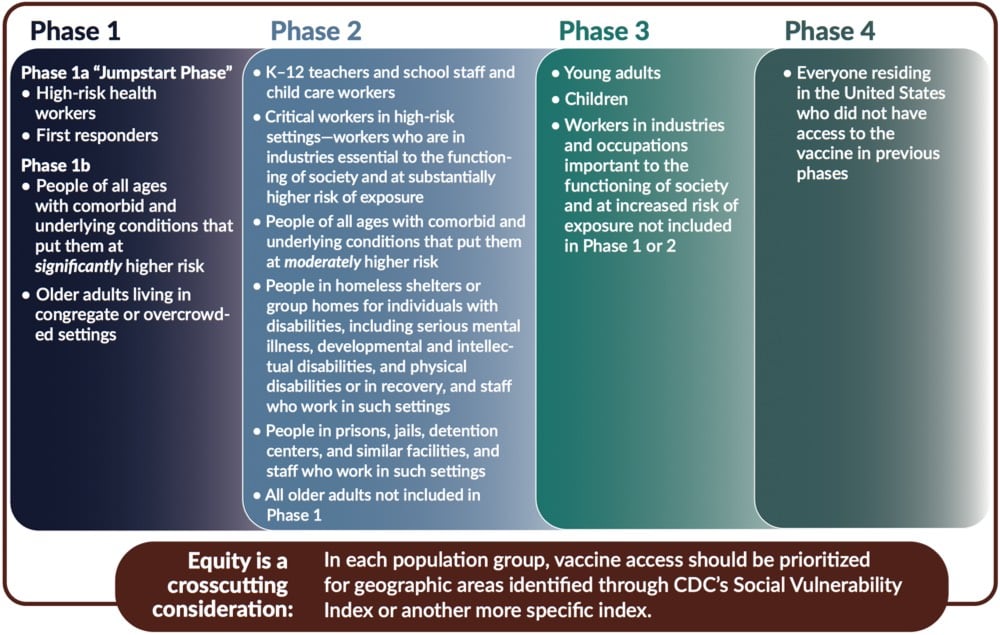
To this end, and in response to a request by the CDC and NIH, the National Academies of Sciences, Engineering, and Medicine formed a committee to produce a report called Framework for Equitable Allocation of COVID-19 Vaccine. The 252-page report is available to the public for free to read online or download.
In addition several recommendations — including that the vaccine be distributed to everyone free of charge — a central feature of the report is a four-phase system of vaccine distribution, summarized in this graphic:
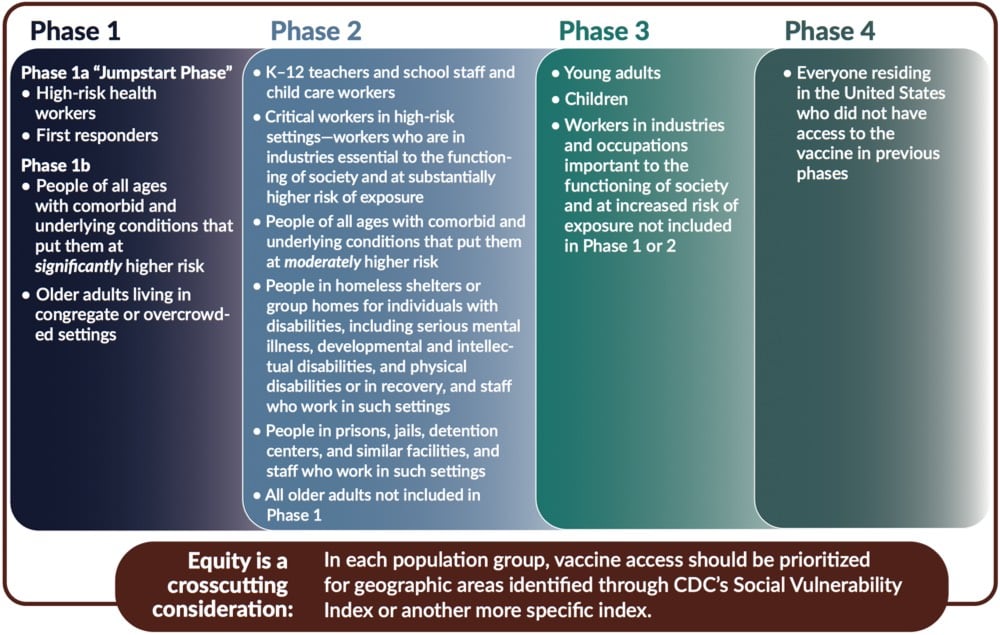
I’d like to stress that this graphic does not show all groups of people included in each phase — please consult the text of the report for that before you go sharing that graphic on social media without context. For example, here’s the full description for “high-risk health workers” in Phase 1a:
This group includes frontline health care workers (who are in hospitals, nursing homes, or providing home care) who either (1) work in situations where the risk of SARS-CoV-2 transmission is higher, or (2) are at an elevated risk of transmitting the infection to patients at higher risk of mortality and severe morbidity. These individuals — who are themselves unable to avoid exposure to the virus — play a critical role in ensuring that the health system can care for COVID-19 patients.
These groups include not only clinicians (e.g., nurses, physicians, respiratory technicians, dentists and hygienists) but also other workers in health care settings who meet the Phase 1a risk criteria (e.g., nursing assistants, environmental services staff, assisted living facility staff, long-term care facility staff, group home staff, and home caregivers). The health care settings employing these workers who are at increased risk of exposure to the virus may also include ambulatory and urgent care clinics; dialysis centers; blood, organ, and tissue donation facilities; and other non-hospital health care facilities. Finally, there are community and family settings where care for infected patients occurs. Not all the workers in these settings are paid for their labor, but, while they are caring for infected people, they all need to be protected from the virus.
Situations associated with higher risk of transmission include caring for COVID-19 patients, cleaning areas where COVID-19 patients are admitted, treated, and housed, and performing procedures with higher risk of aerosolization such as endotracheal intubation, bronchoscopy, suctioning, turning the patient to the prone position, disconnecting the patient from the ventilator, invasive dental procedures and exams, invasive specimen collection, and cardiopulmonary resuscitation. In addition, there are other frontline health care workers who, if they have uncontrolled exposure to the patients or the public in the course of their work, should be in this initial phase. This group includes those individuals distributing or administering the vaccine — especially in areas of higher community transmission — such as pharmacists, plasma and blood donation workers, public health nurses, and other public health and emergency preparedness workers. The committee also includes morticians, funeral home workers, and other death care professionals involved in handling bodies as part of this high-risk group.
The report declines to list specific industries which would be covered in Phase 2’s “critical workers in high-risk settings” but generally says:
The industries in which these critical workers are employed are essential to keeping society and the economy functioning. Since the beginning of the pandemic, millions of people have been going to work and risking exposure to the virus to ensure that markets have food; drug stores have pharmaceutical products; public safety and order are maintained; mail and packages are delivered; and buses, trains, and planes are operating.
Note also the text at the bottom of the graphic: they recommend that within each phase, priority be given to geographic areas where folks are more socially vulnerable in situations like these (e.g. as represented in the CDC’s Social Vulnerability Index).
In developing this phased approach, the committee focused on those who are at the most risk of exposure, severe illness or death, and passing along the virus to others as well as critical workers:
Risk of acquiring infection: Individuals have higher priority to the extent that they have a greater probability of being in settings where SARS-CoV-2 is circulating and of being exposed to a sufficient dose of the virus.
Risk of severe morbidity and mortality: Individuals have higher priority to the extent that they have a greater probability of severe disease or death if they acquire infection.
Risk of negative societal impact: Individuals have higher priority to the extent that societal function and other individuals’ lives and livelihood depend on them directly and would be imperiled if they fell ill.
Risk of transmitting infection to others: Individuals have higher priority to the extent that there is a higher probability of their transmitting the infection to others.
You should read (or at least skim) the full report for more information about the plan and the rationale behind it.
On a personal parting note, as someone who is squarely in the 5-15% of Americans covered in Phase 4 — more specifically: as a 40-something straight white man who non-essentially works from home, isn’t low-income, doesn’t socialize widely even under normal circumstances, and should probably be the very last person on this whole Earth scheduled to be vaccinated under an equitable framework — I am content to wait my turn should the US adopt this framework or something like it.1 Distributing vaccines to those who need them most is absolutely the right thing to do, both ethically and from the standpoint of getting society “back to normal” as quickly as possible and with as little additional death and suffering as possible.
Preliminary results from the trials of the Covid-19 vaccine jointly developed by the University of Oxford and AstraZeneca indicate that the vaccine’s overall efficacy is 70% but that a regimen that calls for a lower first dose is 90% effective.
The preliminary results on the AstraZeneca vaccine were based on a total of 131 Covid-19 cases in a study involving 11,363 participants. The findings were perplexing. Two full doses of the vaccine appeared to be only 62% effective at preventing disease, while a half dose, followed by a full dose, was about 90% effective. That latter analysis was conducted on a small subset of the study participants, only 2,741.
Hopefully more study will be done on that dosage question. From the AP:
“The report that an initial half-dose is better than a full dose seems counterintuitive for those of us thinking of vaccines as normal drugs: With drugs, we expect that higher doses have bigger effects, and more side-effects,” he said. “But the immune system does not work like that.”
The seemingly lower efficacy comes with some perhaps significant benefits: this vaccine is cheaper to produce and doesn’t require any special refrigeration.
The vaccine can be transported under “normal refrigerated conditions” of 2 to 8 degrees Celsius (36 to 46 degrees Fahrenheit), AstraZeneca said. By comparison, Pfizer plans to distribute its vaccine using specially designed “thermal shippers” that use dry ice to maintain temperatures of minus-70 degrees Celsius (minus-94 degrees Fahrenheit).
The Pfizer and Moderna vaccines were pretty similar in many respects and this one seems quite different. These results were just released a few hours ago, so it will be interesting to follow the debate and expert commentary on this. Stay tuned…
Update: This is amazing: the seemingly more effective 1/2 dose + full dose regimen was a mistake.
Around the time when Astra was initiating its partnership with Oxford at the end of April, university researchers were administering doses to trial participants in Britain.
They soon noticed expected side effects such as fatigue, headaches or arm aches were milder than expected, he said.
“So we went back and checked … and we found out that they had underpredicted the dose of the vaccine by half,” said Pangalos.
A far smaller number of participants was given the initial half-dose, so more research will need to be done to determine if this mistake will be added to the long list of scientific discoveries made because of errors. There’s a good piece in Nature that talks about what we know and don’t know about the vaccine results so far along with some informed speculation.
But, if the differences are bona fide, researchers are eager to understand why. “I don’t think it’s an anomaly,” says Katie Ewer, an immunologist at Oxford’s Jenner Institute who is working on the vaccine. “I’m keen to get into the lab and start thinking about how we address that question.” She has two leading theories for why a lower first dose might have led to better protection against COVID. It’s possible that lower doses of vaccine do a better job at stimulating the subset of immune cells called T cells that support the production of antibodies, she says.
Another potential explanation is the immune system’s response against the chimpanzee virus. The vaccine triggers an immune response not only to the SARS-CoV-2 spike protein, but also to components of the viral vector. It’s possible that the full first dose blunted this reaction, says Ewer. She plans to look at antibody responses against the chimpanzee virus to help address this question.
Update: A short thread by Dr. Natalie Dean, which leads with “AstraZeneca/Oxford get a poor grade for transparency and rigor when it comes to the vaccine trial results they have reported”.
For Vox, Julia Belluz takes a look at the approach that’s made Vermont more successful than most other US states in combatting Covid-19. The big thing? State officials recognized that those most at risk needed more support.
There’s a fatal flaw embedded in the basic Covid-19 test, trace, and isolate trifecta used around the world: It doesn’t account for the fact that the coronavirus is not an equal-opportunity pathogen. The people who are most likely to be tested, and to have the easiest time quarantining or isolating, are also the least likely to get sick and die from the virus.
From the United Kingdom to Sweden to Canada, we have evidence that the virus preys on people employed in “essential service” jobs (bus drivers, nurses, factory workers), which don’t allow for telecommuting or paid sick leave; people in low-income neighborhoods; and people in “congregate housing” like shelters, prisons, and retirement homes.
People of color tend to be overrepresented in these groups — but there’s no biological reason they’re more likely to get sick and die from the virus. Simply put: They tend to work jobs that bring them outside the home and into close contact with other people, live in crowded environments ideal for coronavirus contagion, or both.
The state then directed efforts, resources, and money to nursing homes, the unhoused, prisons, and essential workers to make it easier for those folks to stay safe.
I also thought this bit was really interesting:
There’s a simple adage in public health: “Never do a test without offering something in exchange,” said Johns Hopkins’s Stefan Baral. So when a patient gets tested for HIV, for example, they’re offered treatment, support, or contact tracing. “We’re not just doing the testing to get information but also providing a clear service,” Baral added, and potentially preventing that person from spreading the virus any further. “This is basic public health.”
With Covid-19, the US has failed at basic public health. Across the country, people have been asked to get tested without anything offered in exchange.
“If we are asking people to stay home and not work, we have to make sure society is supporting them,” Baral said. “An equitable program would support people to do the right thing.”
“Never do a test without offering something in exchange.” To the extent that federal and state governments have been asking to people to stay home, get tested, and wear a mask, many of those same governments have been unwilling or unable to provide people with much in return for doing so. And so, here we are months into this, paying for that inaction with 250,000 lives.
Update: How NYC does “never do a test without offering something in exchange”:
You can access a free hotel room to safely isolate from your family, which include meals, Rx delivery, free wi-fi, medical staff on site, and transportation to and from hotel and medical appointments.
(via @agoX)
As I write this, it’s snowing outside here in Vermont and Covid-19 has finally gained a foothold in our little state. At the governor’s press conference yesterday, he and his pandemic response team announced that contact tracing done by the state showed that the rise in cases started as an outbreak in some hockey leagues. That initial outbreak wasn’t contained and subsequent non-essential, indoor, mask-less, multi-household gatherings and Halloween parties resulted in the very sharp rise we started to see here in the first week of November.
Scott explained that 71% of outbreaks reported from Oct. 1 to Nov. 13 were linked to “social events, parties and people hanging out at home or bars and clubs.” He added Vermont has not seen the virus spread widely at schools, restaurants or other businesses.
Dr. Mark Levine, the state health commissioner, said those parties came in a variety of sizes of parties — Halloween gatherings large and small, dinner parties, baby showers, “people in the high single numbers at a deer camp.”
In states with many infections, particularly in the Midwest, contact tracing is all but impossible, so it’s instructive to pay attention to Vermont’s example here: we’re doing the tracing and the tracers say the infections are coming from people gathering indoors across multiple households. Which is exactly what public health and medical experts have been urging people not to do for months now.
And that brings us to Thanksgiving. For The Atlantic, Rachel Gutman asked her colleagues who have been writing extensively about the pandemic for some of their top safety rules and guidelines and their number one was, say it with me:
My colleagues’ guidance boils down to this winter’s golden rule for interacting with anyone outside your immediate household: Don’t spend time indoors with other people.
Here it is again in a fun font, just to make sure you got it: 𝓓𝓸𝓷’𝓽 𝓼𝓹𝓮𝓷𝓭 𝓽𝓲𝓶𝓮 𝓲𝓷𝓭𝓸𝓸𝓻𝓼 𝔀𝓲𝓽𝓱 𝓸𝓽𝓱𝓮𝓻 𝓹𝓮𝓸𝓹𝓵𝓮.
Look, for some people spending time indoors with others is essential — jobs, education, etc. — but those who don’t have to, shouldn’t. And this goes for everywhere in the US because no states (aside from maybe Hawaii) are doing well right now — cases are either high, rising sharply, or both. Please please don’t gather in indoor, multi-household groups for Thanksgiving if you haven’t quarantined beforehand. In the US right now, about 1-in-55 people who get Covid-19 die from it. With rates already high around the country, if many people do Thanksgiving as usual, an already horrific and deadly situation could become much much worse.
According to an unpublicized report by the Chinese government, the first documented case of Covid-19 was a 55-year-old person living in Hubei province on November 17, 2019. That makes today the first anniversary of the start of the Covid-19 pandemic. From that person (and possibly earlier or concurrent cases), the disease slowly and silently spread until it was determined to be due to a novel coronavirus.
They found that following the Nov. 17 case, about one to five new cases were reported every day and by Dec. 15, the total infections reached 27. Daily cases seem to have increased after that, with the case count reaching 60 by Dec. 20, the SCMP reported.
On Dec. 27, Dr. Zhang Jixian, head of the respiratory department at Hubei Provincial Hospital, reported to health officials in China that a novel coronavirus was causing the disease; by that day, it had infected more than 180 individuals. (Doctors may not have been aware of all of those cases at the time, but only identified those cases after going back over the records, the Morning Post reported.)
No one had any idea how much the world was going to change that day. What an awful, humbling, terrifying, ghoulish year.
Zeynep Tufekci says that a devastating third pandemic surge is upon us and that It’s Time to Hunker Down. She leads with the good news (vaccines, treatments, knowledge, testing capacity & quickness) but notes that with winter coming and a high baseline of cases from a summer not spent in preparation, now is the time to really knuckle down so that we can get to the finish line.
Whatever the causes, public-health experts knew a fall and winter wave was a high likelihood, and urged us to get ready.
But we did not.
The best way to prepare would have been to enter this phase with as few cases as possible. In exponential processes like epidemics, the baseline matters a great deal. Once the numbers are this large, it’s very easy for them to get much larger, very quickly — and they will. When we start with half a million confirmed cases a week, as we had in mid-October, it’s like a runaway train. Only a few weeks later, we are already at about 1 million cases a week, with no sign of slowing down.
Americans are reporting higher numbers of contacts compared with the spring, probably because of quarantine fatigue and confusing guidance. It’s hard to keep up a restricted life. But what we’re facing now isn’t forever.
It’s time to buckle up and lock ourselves down again, and to do so with fresh vigilance. Remember: We are barely nine or 10 months into this pandemic, and we have not experienced a full-blown fall or winter season. Everything that we may have done somewhat cautiously — and gotten away with — in summer may carry a higher risk now, because the conditions are different and the case baseline is much higher.
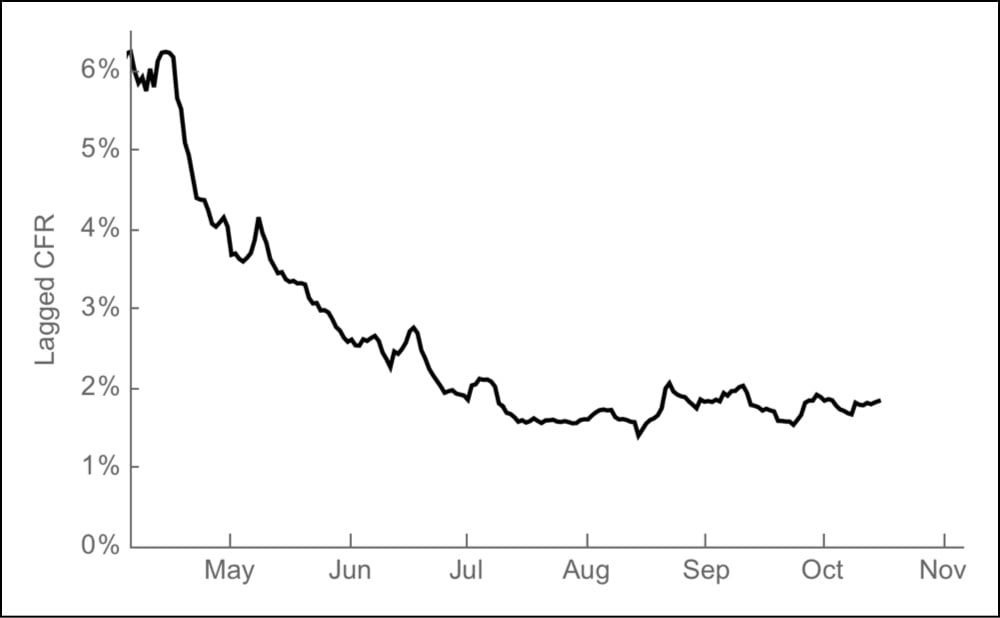
On Friday, November 13, 170,792 new cases of Covid-19 were reported in the United States. About 3000 of those people will die from their disease on Dec 6 — one day of Covid deaths equal to the number of people who died on 9/11. It’s already baked in, it’s already happened. Here’s how we know.
The case fatality rate (or ratio) for a disease is the number of confirmed deaths divided by the number of confirmed cases. For Covid-19 in the United States, the overall case fatality rate (CFR) is 2.3%. That is, since the beginning of the pandemic, 2.3% of those who have tested positive for Covid-19 in the US have died. In India, it’s 1.5%, Germany is at 1.6%, Iran 5.5%, and in Mexico it’s a terrifying 9.8%.
A recent analysis by infectious disease researcher Trevor Bedford tells us two things related to the CFR.
1. Reported deaths from Covid-19 lag behind reported cases by 22 days. Some deaths are reported sooner and some later, but in general it’s a 22-day lag.1
2. The overall CFR in the US is 2.3% but if you use the 22-day lag to calculate what Bedford calls “a lag-adjusted case fatality rate”, it’s a pretty steady average of 1.8% since August. Here’s a graph:
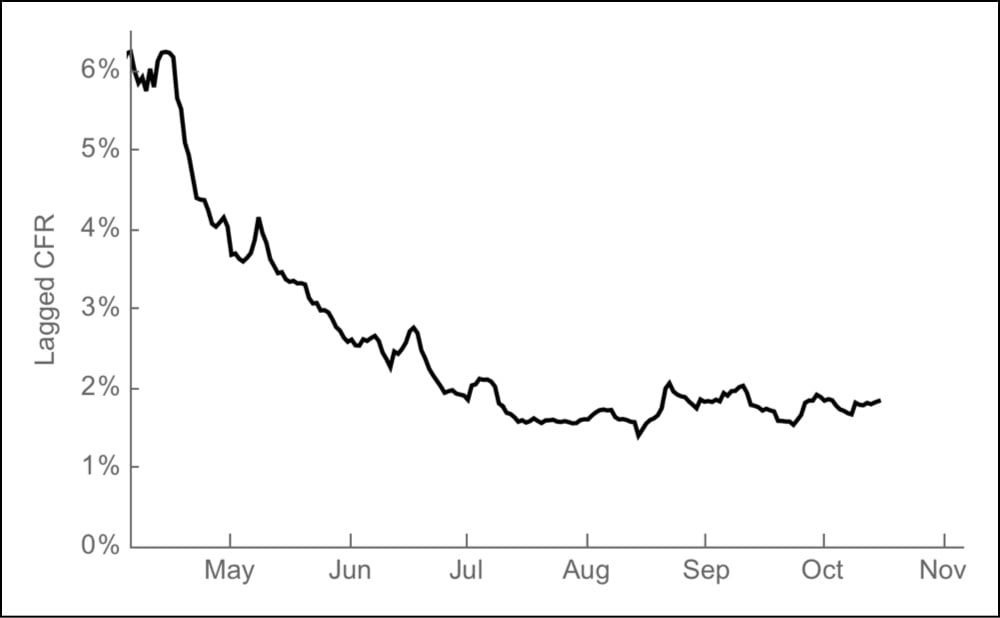
As you can see, in the early days of the pandemic, 4-6% of the cases ended in death and now that’s down to ~1.8%. That’s good news! The less good news is that the current case rate is high and rising quickly. Because of the lag in reported deaths, the rise in cases might not seem that alarming to some, even though those deaths will eventually happen. What Bedford’s analysis provides is a quick way to estimate the number of deaths that will occur in the future based on the number of cases today: just multiply the number of a day’s cases by 1.8% and you get an estimated number of people who will die 22 days later.2
For instance, as I said above, 170,792 cases were reported on Nov 13 — 1.8% is 3074 deaths to be reported on December 6. Cases have been over 100,000 per day for 11 days now: here are the estimated deaths from that time period:
| Date |
Cases |
Est. deaths (on date) |
| 2020-11-15 | 145,670 | 2622 (2020-12-08) |
| 2020-11-14 | 163,473 | 2943 (2020-12-07) |
| 2020-11-13 | 170,792 | 3074 (2020-12-06) |
| 2020-11-12 | 150,526 | 2709 (2020-12-05) |
| 2020-11-11 | 144,499 | 2601 (2020-12-04) |
| 2020-11-10 | 130,989 | 2358 (2020-12-03) |
| 2020-11-09 | 118,708 | 2137 (2020-12-02) |
| 2020-11-08 | 110,838 | 1995 (2020-12-01) |
| 2020-11-07 | 129,191 | 2325 (2020-11-30) |
| 2020-11-06 | 125,252 | 2255 (2020-11-29) |
| 2020-11-05 | 116,153 | 2091 (2020-11-28) |
| 2020-11-04 | 103,067 | 1855 (2020-11-27) |
| Totals | 1,609,158 | 28,965 |
Starting the day after Thanksgiving, a day traditionally called Black Friday, the 1.6 million positive cases reported in the past 12 days will result in 2-3000 deaths per day from then into the first week of December. Statistically speaking, these deaths have already occurred — as Bedford says, they are “baked in”. Assuming the lagged CFR stays at ~1.8% (it could increase due to an overtaxed medical system) and if the number of cases keeps rising, the daily death toll would get even worse. As daily case totals are reported, you can just do the math yourself:
number of cases × 0.018
200,000 cases in a day would be ~3600 deaths. 300,000 daily cases, a number that would have been inconceivable to imagine in May but is now within the realm of possibility, would result in 5400 deaths in a single day. Vaccines are coming, there is hope on the horizon. But make no mistake: this is an absolute unmitigated catastrophe for the United States.
Update: Over at The Atlantic, Alexis Madrigal and Whet Moser took a closer look at Bedford’s model, aided by Ryan Tibshirani’s analysis.
Tibshirani’s first finding was that the lag time between states was quite variable-and that the median lag time was 16 days, a lot shorter than the mean. Looking state by state, Tibshirani concluded, it seemed difficult to land on an exact number of days as the “right” lag “with any amount of confidence,” he told us. Because cases are rising quickly, a shorter lag time would mean a larger denominator of cases for recent days — and a lower current case-fatality rate, something like 1.4 percent. This could mean fewer overall people are dying.
But this approach does not change the most important prediction. The country will still cross the threshold of 2,000 deaths a day, and even more quickly than Bedford originally predicted. Cases were significantly higher 16 days ago than 22 days ago, so a shorter lag time means that those higher case numbers show up in the deaths data sooner. Even with a lower case-fatality rate, deaths climb quickly. Estimating this way, the country would hit an average of 2,000 deaths a day on November 30.
The other major finding in Tibshirani’s analysis is that the individual assumptions and parameters in a Bedford-style model don’t matter too much. You can swap in different CFRs and lag-time parameters, and the outputs are more consistent than you might expect. They are all bad news. And, looking retrospectively, Tibshirani found that a reasonable, Bedford-style lagged-CFR model would have generated more accurate national-death-count predictions than the CDC’s ensemble model since July.
Last Monday the world got some good news: an early review of the data showed that Pfizer’s Covid-19 vaccine was “more than 90% effective” in preventing the disease. The results pointed to other vaccines also being highly effective against the virus and this morning comes this news: Early Data Show Moderna’s Coronavirus Vaccine Is 94.5% Effective.
The drugmaker Moderna announced on Monday that its coronavirus vaccine was 94.5 percent effective, based on an early look at the results from its large, continuing study.
Researchers said the results were better than they had dared to imagine. But the vaccine will not be widely available for months, probably not until spring.
Despite the delivery timeline, this is such good news.
The companies’ products open the door to an entirely new way of creating vaccines — and creating them fast. Both use a synthetic version of coronavirus genetic material, called messenger RNA or mRNA, to program a person’s cells to churn out many copies of a fragment of the virus. That fragment sets off alarms in the immune system and stimulates it to attack, should the real virus try to invade. Although a number of vaccines using this technology are in development for other infections and cancers, none have yet been approved or marketed.
“The fact that two different vaccines made by two different companies with two different kinds of structures, in a new messenger RNA concept, both worked so effectively confirms the concept once and for all that this is a viable strategy not only for Covid but for future infectious disease threats,” said Dr. Barry R. Bloom, a professor of public health at Harvard.
Natalie E. Dean, a biostatistician at the University of Florida, said an important finding was that the vaccine appeared to prevent severe disease. Pfizer did not release information about disease severity when reporting its results.
Researchers say the positive results from Pfizer and Moderna bode well for other vaccines, because all of the candidates being tested aim at the same target - the so-called spike protein on the coronavirus that it uses to invade human cells.
It’s only a few more months — please please do what you can to stay safe and keep others safe (especially medical workers) until these vaccines can be rolled out.
In a press release (and not a paper in a peer-reviewed journal) based on a preliminary outside review of data from its phase 3 trial, Pfizer says its Covid-19 vaccine was more than 90% effective in preventing the disease.
The company said that the analysis found that the vaccine was more than 90 percent effective in preventing the disease among trial volunteers who had no evidence of prior coronavirus infection. If the results hold up, that level of protection would put it on par with highly effective childhood vaccines for diseases such as measles. No serious safety concerns have been observed, the company said.
I really hope this analysis holds up when more data from the study is released:
The data released by Pfizer Monday was delivered in a news release, not a peer-reviewed medical journal. It is not conclusive evidence that the vaccine is safe and effective, and the initial finding of more than 90 percent efficacy could change as the trial goes on.
The world, and the United States, could really really use some good news like this about the pandemic.
Update: Here’s Pfizer’s press release. And a thread from Dr. Natalie Dean on how she is interpreting this news (“Celebrate, but let the process play out over time as intended.”)
Pfizer’s first analysis was planned for 32 events, which they pushed back after discussions with FDA. But by the time they analyzed the data, 94 had accrued. This shows how quickly trials can generate results when placed in hotspots (and how much transmission is ongoing!).
These vaccines are tested until a certain number of infections happen. So you have this interesting paradoxical situation where if a potential vaccine is more successful at curbing infection, the longer it takes for the study to conclude. You get a better vaccine but wait longer for it. Countering that are the rising transmission counts in the US — more community transmission will get you to the target number of infections more quickly.
Update: From virologist Dr. Florian Krammer, a thread about what Pfizer and other companies will be looking for in terms of the efficacy of vaccines in a number of different situations. Overall, he is optimistic about these preliminary results. And here’s a FAQ about the vaccine from the NY Times.
Another open question is whether children will get protection from the vaccine. The trial run by Pfizer and BioNTech initially was open to people 18 or older, but in September they began including teenagers as young as 16. Last month, they launched a new trial on children as young as 12 and plan to work their way to younger ages.
Update: A very simplified explanation of Pfizer’s RNA-based vaccine.
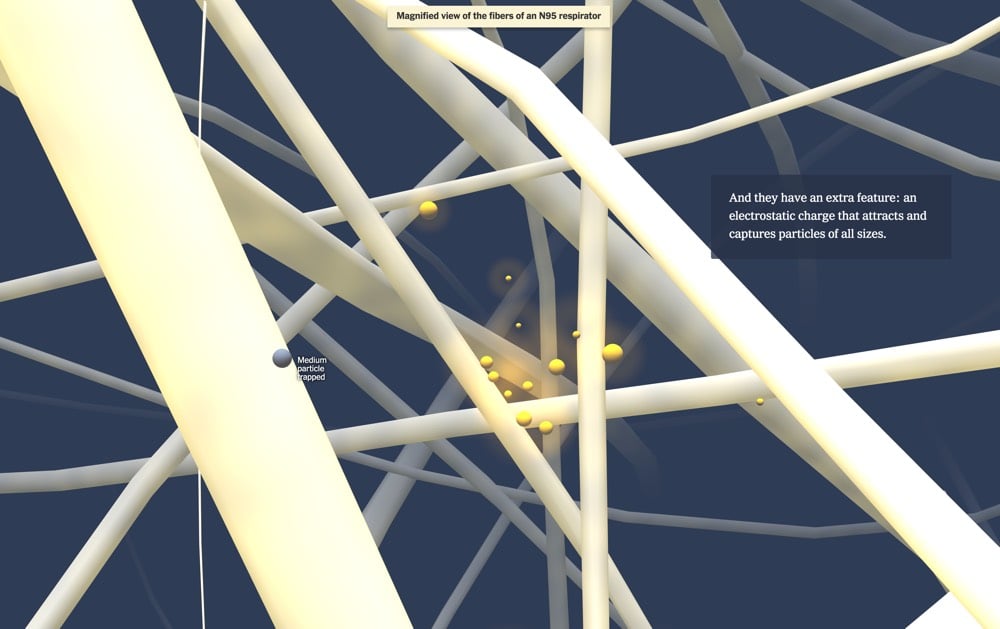
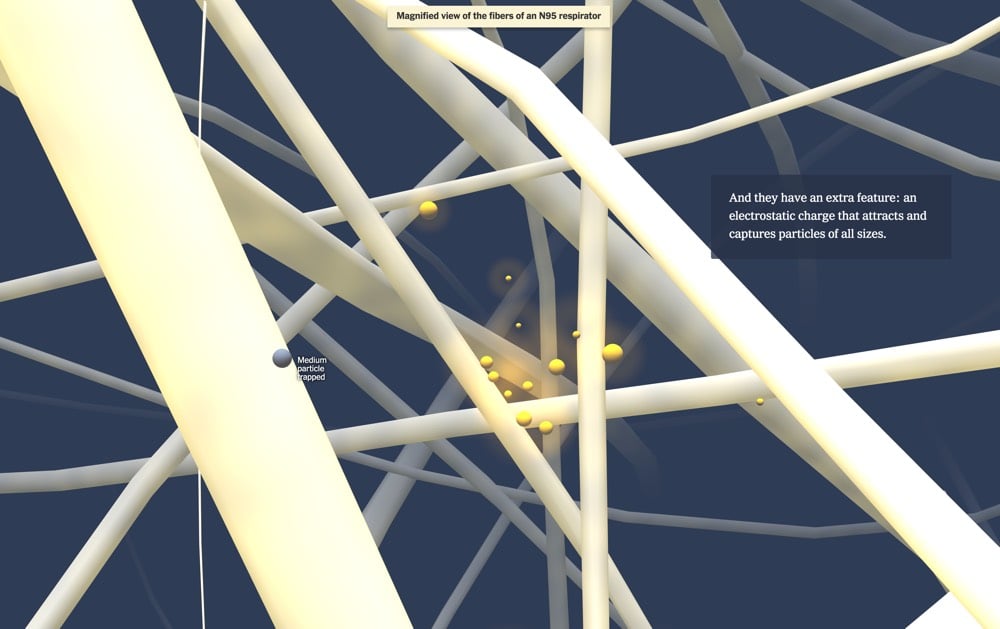
The NY Times has a fantastic visualization on how face masks help keep us safe from catching Covid-19 by taking readers on a journey through a mask to see how they block aerosols and droplets.
A lot of the pushback around the efficacy of masks from non-scientists focuses on the size of the droplets and aerosols (super tiny) compared to the gaps between the fibers in the masks (relatively large). Intuitively, it seems like masks don’t stand a chance of stopping anything. But as this visualization shows, multiple layers of fibers do the job quite well. Masks don’t work like sieves, which will let every particle smaller than the holes through the mesh. Instead, imagine shooting a BB gun into a thick stand of trees — no one tree stands a good chance of getting hit by the BB but the forest will stop it eventually.
N95, KN95, and masks made from polypropylene have an extra weapon against particles: the fibers carry an electrostatic charge that attracts particles to trap them. Picture our BB flying through a forest of magnetic trees — it’s got a much better chance of being captured that way.
The visualization also touches on the importance of making sure your mask fits properly. The best masks fit tightly around the edges and include a space around your nose and nostrils. Masks with unfiltered valves should not be used — you’re just breathing virus out into the air. It’s been 8-9 months now that we’ve been dealing with the pandemic and there will be many more months of wearing masks. If your mask is fits poorly around your nose, your straps aren’t tight enough, you need to fuss with it after putting it on, have a mask with a valve, or (god forbid) are still just wearing a bandana, please please do yourself and others a favor and upgrade your mask. High-quality, well-made masks are much easier to find now than 6-8 months ago.1 If you can’t afford a proper mask, email me and I’ll buy you one. Masks are one of the most successful low-tech interventions we can do to prevent the spread of Covid-19, and the better our masks, the more effective they will be.
A spin studio (aka an indoor gym with stationary bikes) in Hamilton, Ontario is dealing with an outbreak of Covid-19 stemming from one asymptomatic patron that has resulted in 69 positive cases so far, even though the studio “followed the rules”. From the CNN report:
SPINCO, in Hamilton, Ontario, just reopened in July and had all of the right protocols in place, including screening of staff and attendees, tracking all those in attendance at each class, masking before and after classes, laundering towels and cleaning the rooms within 30 minutes of a complete class, said Dr. Elizabeth Richardson, Hamilton’s medical officer of health, in a statement.
As the Washington Post reports, patrons were allowed to take their masks off while exercising:
Although Hamilton requires masks to be worn in most public settings, the law includes an exemption for anyone “actively engaged in an athletic or fitness activity.” In keeping with that policy, the studio, SPINCO, allowed riders to remove their masks once clipped into their bikes, and told them to cover up again before dismounting.
The problem here is that while the studio may have followed the rules, they were not the right rules. This outbreak appears to be another clear-cut instance of Covid-19 spread by aerosols. A group of people indoors, without masks, breathing heavily, over long periods of time in what I’m guessing is not a properly ventilated room — this is exactly the sort of thing that has been shown over and over again to be problematic.1 The science is there, but governments and public health agencies have not caught up with this yet. If you take the transmission by aerosols into account, the rules for gyms (and bars and restaurants) being open is that they should probably not be open at all — or if they are, they should be well-ventilated and the wearing of masks should be mandatory at all times.2 (via @DrEricDing)
We’re all so goddamned tired of this fucking pandemic and so people are looking at the development and distribution of a vaccine as the thing that’s going to get us out of this (and quick). But realistically, that’s not what’s going to happen. Carl Zimmer wrote about some of the challenges with Covid-19 vaccines.
The first vaccines may provide only moderate protection, low enough to make it prudent to keep wearing a mask. By next spring or summer, there may be several of these so-so vaccines, without a clear sense of how to choose from among them. Because of this array of options, makers of a superior vaccine in early stages of development may struggle to finish clinical testing. And some vaccines may be abruptly withdrawn from the market because they turn out not to be safe.
“It has not yet dawned on hardly anybody the amount of complexity and chaos and confusion that will happen in a few short months,” said Dr. Gregory Poland, the director of the Vaccine Research Group at the Mayo Clinic.
See also Dr. Fauci’s belief that our best case scenario for returning to something close to normal life in the US is late 2021.
On Twitter, Zimmer also commented on something that I hadn’t really thought about: that all of these vaccines in development in the US are only for adults:
I wrote last month that no trials for kids had started. Update: still no US trials for kids. The goal of having shots ready for them by fall 2021 may be slipping further away.
From Zimmer’s article on the development of a kids’ vaccine:
Only if researchers discovered no serious side effects would they start testing them in children, often beginning with teenagers, then working their way down to younger ages. Vaccine developers are keenly aware that children are not simply miniature adults. Their biology is different in ways that may affect the way vaccines work. Because their airways are smaller, for example, they can be vulnerable to low levels of inflammation that might be harmless to an adult.
These trials allow vaccine developers to adjust the dose to achieve the best immune protection with the lowest risk of side effects. The doses that adults and children need are sometimes different — children get smaller doses of hepatitis B vaccines, for example, but bigger doses for pertussis.
You probably hate reading these kinds of articles; I know I do. But facing up to the reality of our situation, particularly here in the US where our political leadership has utterly failed in protecting us from this virus, is much better than burying our heads in the sand — that’s just not mentally healthy.
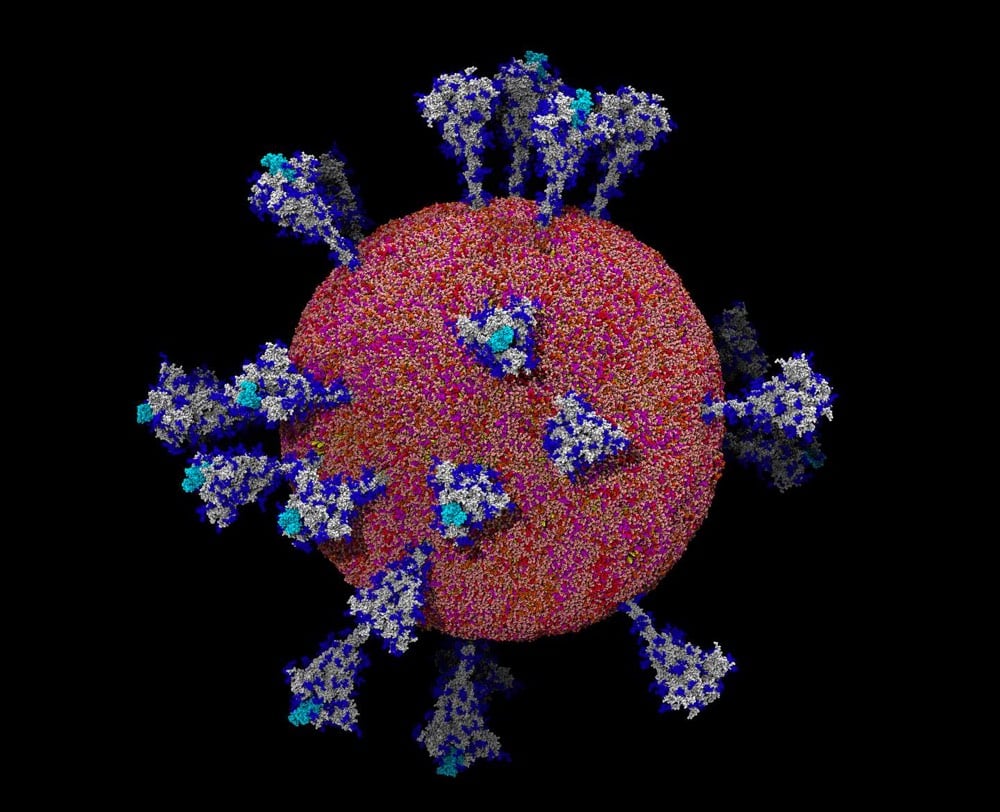
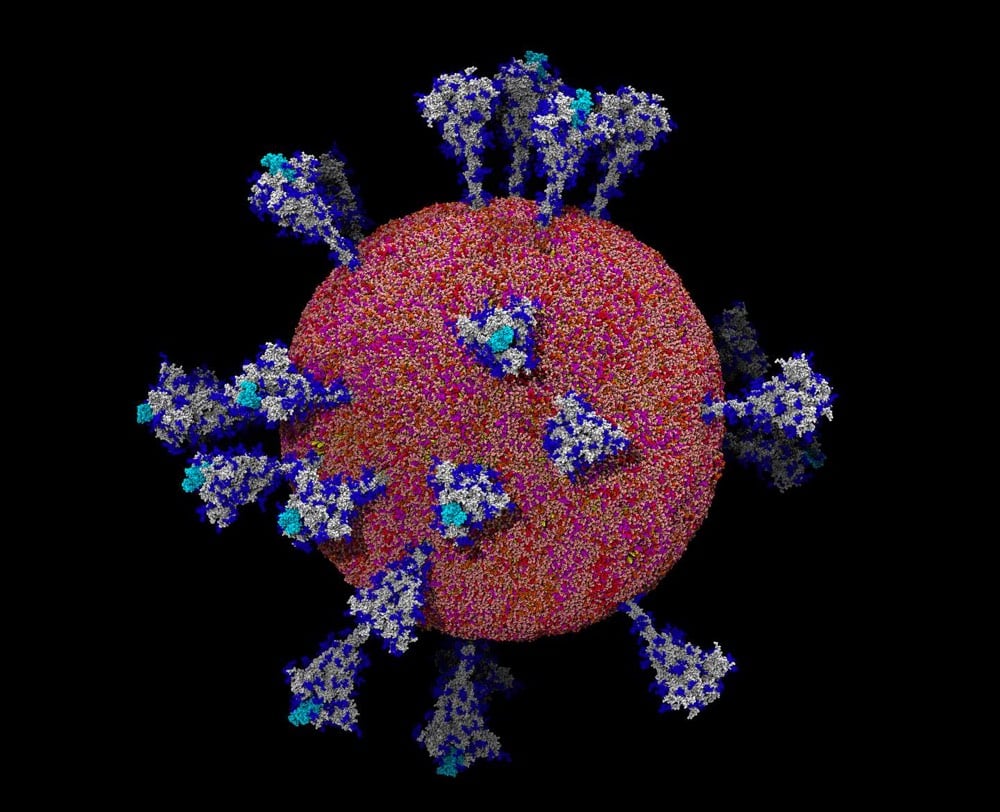
This is a great piece from Carl Zimmer about how much scientists have learned about SARS-CoV-2 through imaging, including how the virus works and prospects for treatment and a vaccine.
Thanks to the work of scientists like Dr. Li, the new coronavirus, known as SARS-CoV-2, is no longer a cipher. They have come to know it in intimate, atomic detail. They’ve discovered how it uses some of its proteins to slip into cells and how its intimately twisted genes commandeer our biochemistry. They’ve observed how some viral proteins throw wrenches into our cellular factories, while others build nurseries for making new viruses. And some researchers are using supercomputers to create complete, virtual viruses that they hope to use to understand how the real viruses have spread with such devastating ease.
I’ve been watching the lectures for MIT’s online Covid-19 class and the thing that has struck me most is just how much scientists have learned about the SARS-CoV-2 virus in such a short amount of time. To be clear, there are many things that they still do not understand about it (and viruses in general), but scientists know this thing upside down and backwards. The depth and breadth of their knowledge is so impressive and I wish more people were aware of it.
A few weeks ago during the Q&A session after his lecture for MIT’s online biology class about the pandemic, Dr. Anthony Fauci shared his expert opinion on when things might return to “normal” in the US. Here was my paraphrased tweet about it:
With a very effective vaccine ready in Nov/Dec, distributed widely, and if lots of people take it (i.e. the best case scenario), the earliest we could return to “normal life” in the world is the end of 2021.
At the New Yorker Festival earlier in the week, Michael Specter asked him about a return to normalcy and Fauci elaborated a bit more on this timeline (starts ~10:22 in the video).
When are we gonna get back to something that closely resembles, or is in fact, normal as we knew it?
We’re already making doses, tens and hundreds of millions of doses to be ready, first at least, in graded numbers at the end of the year in November/December. By the time we get to April, we likely will have doses to be able to vaccinate anybody who needs to be vaccinated. But logistically by the time you get everybody vaccinated, it likely will not be until the third or even the beginning of the fourth quarter of 2021.
So let’s say we get a 70% effective vaccine, which I hope we will get, but only 60% of the people get vaccinated. There are going to be a lot of vulnerable people out there, which means that the vaccine will greatly help us to pull back a bit on the restrictions that we have now to maintain good public health, but it’s not going to eliminate things like mask wearing and avoiding crowds and things like that.
So I think we can approach normality, but I don’t think we’re going to be back to normal until the end of 2021. We may do better than that; I hope so but I don’t think so.
Leaving aside what “normal” might mean and who it actually applies to,1 there’s some good news and bad news in there. The good news is, they’re already producing doses of the vaccine to be ready if and when the phase 3 trials are successful. Ramping up production before the trials conclude isn’t usually done because it’s a waste of money if the trials fail, but these vaccines are so critical to saving lives that they’re spending that money to save time. That’s great news.
The bad news is that we’re not even halfway through the pandemic in the best case scenario. We’re going to be wearing masks in public for at least another year (and probably longer than that). Large gatherings of people (especially indoors) will continue to be problematic — you know: movie theaters, concerts, clubs, bars, restaurants, schools, and churches — and folks staying within small pods of trusted folks will likely be the safest course of action.
A change in national leadership in both the executive branch and Senate could change the outlook for the better. We could get some normalcy back even without a vaccine through measures like a national mask mandate/distribution, a real national testing & tracing effort, taking aerosol transmission seriously, and easing the economic pressure to “open back up” prematurely. We’re never going to do as well as Vietnam or Taiwan, but I’d settle for Greece or Norway.
Update: In an interview posted yesterday, Johns Hopkins epidemiologist Dr. Caitlin Rivers gives her best guess at a return to normalcy:
Topol: When do you think we’ll see pre-COVID life restored?
Rivers: I wish I knew. I’m thinking toward the end of 2021. It’s really hard to say with any certainty. We should all be mentally prepared to have quite a bit ahead of us.
Back in June, in a post called Jesus Christ, Just Wear a Face Mask!, I presented a bunch of evidence and arguments for wearing face masks to prevent the spread of Covid-19. Even then it was pretty clear that masks were working. In piece published by Nature yesterday, Lynne Peeples summarizes what the data and science currently says about the effectiveness of wearing face masks. Here is her one-sentence summary:
To be clear, the science supports using masks, with recent studies suggesting that they could save lives in different ways: research shows that they cut down the chances of both transmitting and catching the coronavirus, and some studies hint that masks might reduce the severity of infection if people do contract the disease.
And importantly, even ardently pro-mask scientists agree that masks should be worn in conjunction with taking other precautions: limiting large gatherings, maintaining distance, limiting the time you spend indoors with others, etc.
In secrecy over the past several months, filmmaker Alex Gibney has been making a documentary film about the US government’s response to the Covid-19 pandemic called Totally Under Control. He and co-directors Ophelia Harutyunyan and Suzanne Hillinger interviewed “countless scientists, medical professionals, and government officials on the inside” to produce the film.
Academy Award-winning filmmaker Alex Gibney, directing with Ophelia Harutyunyan and Suzanne Hillinger, interrogates this question and its devastating implications in Totally Under Control. With damning testimony from public health officials and hard investigative reporting, Gibney exposes a system-wide collapse caused by a profound dereliction of Presidential leadership.
Gibney previously directed Enron: The Smartest Guys in the Room, Going Clear, and Zero Days (all excellent documentaries). The film comes out in theaters on October 13 and on Hulu on October 20.
A group of scientists who believe that WHO and the CDC are being too slow in acknowledging the role of aerosol transmission in spreading Covid-19 have written up a Google Doc of advice for the public: FAQs on Protecting Yourself from COVID-19 Aerosol Transmission.
The goal of these FAQs is to provide information to the general public in an efficient manner about how to prevent aerosol transmission of COVID-19, with the hope that this will allow more informed decision making by individuals or organizations. All of this information has been posted in Twitter and other forums, but can be difficult to find. Having multiple experts working together, and having the ability to update this information also improves its quality. These FAQs represent our best understanding at this time, and should always be similar or more stringent than information provided by CDC, WHO, and most regional & local health authorities. If your authority has a more stringent guideline than discussed here, follow that more stringent guideline.
The group was organized by chemist Jose-Luis Jimenez, who has been studying aerosols for 20 years. You may remember Jimenez from his excellent piece in Time magazine, where he used the analogy of smoke to explain aerosol transmission. Here’s a snippet from the FAQ, highlighting something I’ve been concerned about lately: people wearing face shields instead of masks and employees in stores not wearing masks behind plexiglass shields:
7.13. Are face shields and masks interchangeable?
No, face shields do not offer much protection against aerosols (also see this video), while masks do. Face shields are good for blocking ballistic droplets released by the wearer or that might fly into the wearer’s face when close to others. Face shields are considered a supplement to masks for partial eye protection (but less useful than closed glasses, as discussed above), but not a substitute for them.
7.14. Are plexiglass barriers helpful?
Plexiglass barriers are generally useful to avoid direct droplet infection and direct aerosol transmission whenever people are in close proximity and distance cannot be kept. Therefore, it is recommended to use them as a direct transmission suppression tool at such places, such as a supermarket checkout.
However, as aerosols follow the air movements indoors, the protective effects of the plexiglas barriers against aerosols will be limited. Plexiglas barriers alone are not a sufficient approach to protect against aerosol transmission. Their installation alone cannot protect against indoor aerosol transmission and should not be regarded as safe and sufficient protection.
MIT Technology Review’s Charlotte Jee interviewed Jimenez about the FAQ document.
We update the document all the time. We’re effectively having to be a little WHO or CDC. We’re saying the things that they should be saying. This is frustrating, but it’s the situation we find ourselves in. These organizations have been flat-out refusing to consider if aerosol transmission is important, which leaves people unprotected. So we feel it’s our duty to communicate directly with the public.
Right now, in my opinion as someone who has done a ton of reading about Covid-19, the most best accessible information on how individuals and societies can protect themselves and others during the pandemic (and why) is available in Jimenez’s Time article, Aaron Carroll’s NY Times piece about how to think about risk management, Zeynep Tufekci’s piece in the Atlantic about dispersion and superspreading, and now this Google Doc by Jimenez et al.
Zeynep Tufekci says that we are paying too much attention to the R value of SARS-CoV-2 (basically the measure of its contagiousness) and not nearly enough attention to the k value (“whether a virus spreads in a steady manner or in big bursts, whereby one person infects many, all at once”).
There are COVID-19 incidents in which a single person likely infected 80 percent or more of the people in the room in just a few hours. But, at other times, COVID-19 can be surprisingly much less contagious. Overdispersion and super-spreading of this virus is found in research across the globe. A growing number of studies estimate that a majority of infected people may not infect a single other person. A recent paper found that in Hong Kong, which had extensive testing and contact tracing, about 19 percent of cases were responsible for 80 percent of transmission, while 69 percent of cases did not infect another person. This finding is not rare: Multiple studies from the beginning have suggested that as few as 10 to 20 percent of infected people may be responsible for as much as 80 to 90 percent of transmission, and that many people barely transmit it.
We’ve known, or at least suspected, this about SARS-CoV-2 for awhile now — I linked to two articles about superspreading back in May and June — but Tufekci says we have not adjusted our thinking about what that means for prevention. We should be avoiding superspreading environments/events (“Avoid Crowding, Indoors, low Ventilation, Close proximity, long Duration, Unmasked, Talking/singing/Yelling”), doing backwards contact tracing, and rapid testing.
In an overdispersed regime, identifying transmission events (someone infected someone else) is more important than identifying infected individuals. Consider an infected person and their 20 forward contacts-people they met since they got infected. Let’s say we test 10 of them with a cheap, rapid test and get our results back in an hour or two. This isn’t a great way to determine exactly who is sick out of that 10, because our test will miss some positives, but that’s fine for our purposes. If everyone is negative, we can act as if nobody is infected, because the test is pretty good at finding negatives. However, the moment we find a few transmissions, we know we may have a super-spreader event, and we can tell all 20 people to assume they are positive and to self-isolate-if there is one or two transmissions, it’s likely there’s more exactly because of the clustering behavior. Depending on age and other factors, we can test those people individually using PCR tests, which can pinpoint who is infected, or ask them all to wait it out.
Part of the problem is that dispersion and its effects aren’t all that intuitive.
Overdispersion makes it harder for us to absorb lessons from the world because it interferes with how we ordinarily think about cause and effect. For example, it means that events that result in spreading and non-spreading of the virus are asymmetric in their ability to inform us. Take the highly publicized case in Springfield, Missouri, in which two infected hairstylists, both of whom wore masks, continued to work with clients while symptomatic. It turns out that no apparent infections were found among the 139 exposed clients (67 were directly tested; the rest did not report getting sick). While there is a lot of evidence that masks are crucial in dampening transmission, that event alone wouldn’t tell us if masks work. In contrast, studying transmission, the rarer event, can be quite informative. Had those two hairstylists transmitted the virus to large numbers of people despite everyone wearing masks, it would be important evidence that, perhaps, masks aren’t useful in preventing super-spreading.
The piece is an important read and interesting throughout: just read the whole thing.
A coalition of organizations led by Project South (which was founded as the Institute to Eliminate Poverty & Genocide — more on that last word in a minute) has filed a complaint based on a whistleblower about an ICE concentration camp in Georgia where, the complaint alleges, detained immigrants are not being properly treated for Covid-19, important medications are being withheld, conditions are appalling, and women are being given unnecessary hysterectomies. From a piece about the complaint:
Multiple women came forward to tell Project South about what they perceived to be the inordinate rate at which women in ICDC were subjected to hysterectomies — a surgical operation in which all or part of the uterus is removed. Additionally, many of the immigrant women who underwent the procedure were reportedly “confused” when asked to explain why they had the surgery, with one detainee likening their treatment to prisoners in concentration camps.
“Recently, a detained immigrant told Project South that she talked to five different women detained at ICDC between October and December 2019 who had a hysterectomy done,” the complaint stated. “When she talked to them about the surgery, the women ‘reacted confused when explaining why they had one done.’ The woman told Project South that it was as though the women were ‘trying to tell themselves it’s going to be OK.’”
“When I met all these women who had had surgeries, I thought this was like an experimental concentration camp. It was like they’re experimenting with our bodies,” the detainee said.
According to Wooten, ICDC consistently used a particular gynecologist — outside the facility — who almost always opted to remove all or part of the uterus of his female detainee patients.
“Everybody he sees has a hysterectomy — just about everybody,” Wooten said, adding that, “everybody’s uterus cannot be that bad.”
According to the UN’s Genocide Convention of 1948, “imposing measures intended to prevent births” within “a national, ethnical, racial or religious group” is genocide. Congresswoman Alexandria Ocasio-Cortez commented:
The fact of the matter is the United States has engaged in a program of mass human rights violations targeting immigrants.
I’ll remind you, as I have with increasing frequency lately about the activities of our country’s increasingly authoritarian government, that forced sterilization in detention camps is literally what the literal Nazis did (inspired by, you guessed it, America’s treatment of “undesirable” populations).
You can read the complaint here and check out this thread from Brooke Binkowski for more context and examples of detainee mistreatment at the hands of the increasingly extra-legal ICE.
I’ve never read or seen any of the Dunes (Herbert’s book, David Lynch’s movie, or even Jodorowsky’s Dune) but I have very fond memories of the video game Dune II and will watch anything that Denis Villeneuve makes, so I’m definitely going to check this out when it’s released…let’s see….on December 18, 2020 in theaters? WTF?
Ok, so just watch the trailer if that’s what you’re here for, but I remain baffled that movie theaters are a) currently open (Tenet was showing in 2810 US theaters last weekend) and b) slated to still be open in December in a country trapped in a pandemic death spiral. Easy testing w/ quick results and contact tracing, the twin keys to controlling the virus, are still a mess. A safe & tested vaccine that’s distributed widely by the end of the year? I wouldn’t hold my breath. And you’re going to put a bunch of people who are laughing and gasping together in a room for two-plus hours with a virus that’s airborne1 and assume they’re going to stay properly masked up (except for when they are eating popcorn and nachos!) and properly distant from each other? (Have you met Americans?!) Even if you assume that movie theater screening rooms are huge & well-ventilated (some definitely are not) and capacity is restricted, I repeat: What The Fuck? And in terms of societal trade-offs, reopening places where people gather indoors for entertainment is more important than ensuring our kids can safely go to school? *extreme hair-tearing-out noise*
Update: Aaaaand the Dune release has been delayed until Oct 2021. Between the Trump debacle2 and the CDC acknowledging that the virus may spread through aerosols, I feel like people are coming around to the idea that indoor gatherings, entertainment, and dining are going to be problematic for several more months.
Chemist Jose-Luis Jimenez writing for Time magazine: COVID-19 Is Transmitted Through Aerosols. We Have Enough Evidence, Now It Is Time to Act. In it, he argues that while much of the early attention has been on fomites (surface contamination) and droplets as pathways for spreading Covid-19, tranmission by aerosols may be more significant. His analogy of smoke makes it quite easy to understand:
When it comes to COVID-19, the evidence overwhelmingly supports aerosol transmission, and there are no strong arguments against it. For example, contact tracing has found that much COVID-19 transmission occurs in close proximity, but that many people who share the same home with an infected person do not get the disease. To understand why, it is useful to use cigarette or vaping smoke (which is also an aerosol) as an analog. Imagine sharing a home with a smoker: if you stood close to the smoker while talking, you would inhale a great deal of smoke. Replace the smoke with virus-containing aerosols, which behave very similarly, and the impact is similar: the closer you are to someone releasing virus-carrying aerosols, the more likely you are to breathe in larger amounts of virus. We know from detailed, rigorous studies that when individuals talk in close proximity, aerosols dominate transmission and droplets are nearly negligible.
Thinking of smoke can help guide our actions:
The visual analogy of smoke can help guide our risk assessment and risk reduction strategies. One just has to imagine that others they encounter are all smoking, and the goal is to breathe as little smoke as possible. But COVID-19 is not very contagious under most situations, unlike, for example, measles: the CDC says that 15 minutes of close proximity to a COVID-19 infected person often leads to contagion, which provides an estimate of how much “exhaled smoke” one may need to inhale for infection. Inhaling a little whiff of “smoke” here and there is OK, but a lot of “smoke” for a sustained period of time and without a mask is risky. (To be clear, actual smoke does not increase the probability of infection.)
In thinking about aerosolized Covid, Jimenez recommends avoiding crowds & indoor spaces and cutting down on proximity & duration, among other things.
We should continue doing what has already been recommended: wash hands, keep six feet apart, and so on. But that is not enough. A new, consistent and logical set of recommendations must emerge to reduce aerosol transmission. I propose the following: Avoid Crowding, Indoors, low Ventilation, Close proximity, long Duration, Unmasked, Talking/singing/Yelling (“A CIViC DUTY”). These are the important factors in mathematical models of aerosol transmission, and can also be simply understood as factors that impact how much “smoke” we would inhale.
But what about masks? N95s can block most aerosols but cloth masks have “huge” holes in them relative to aerosol particles, right? They still work in lowering risk (but not eliminating it!) because your “smoke” doesn’t travel as far when you’re wearing a mask and it filters incoming smoke (if your mask fits correctly and you’re keeping your distance).
Second, masks are essential, even when we are able to maintain social distance. We should also pay attention to fitting masks snugly, as they are not just a parapet against ballistic droplets, but also a means to prevent “smoke” from leaking in through gaps. We should not remove masks to talk, nor allow someone who is not wearing a mask to talk to us, because we exhale aerosols 10 times as much when talking compared to breathing. Everyone should be careful to not stand behind someone with a poorly fitting mask, as the curvature of an ill-fitting mask can cause aerosols to travel behind the person wearing it.
Great article, full of common sense advice backed up by science.
Newer posts
Older posts




Socials & More