kottke.org posts about medicine
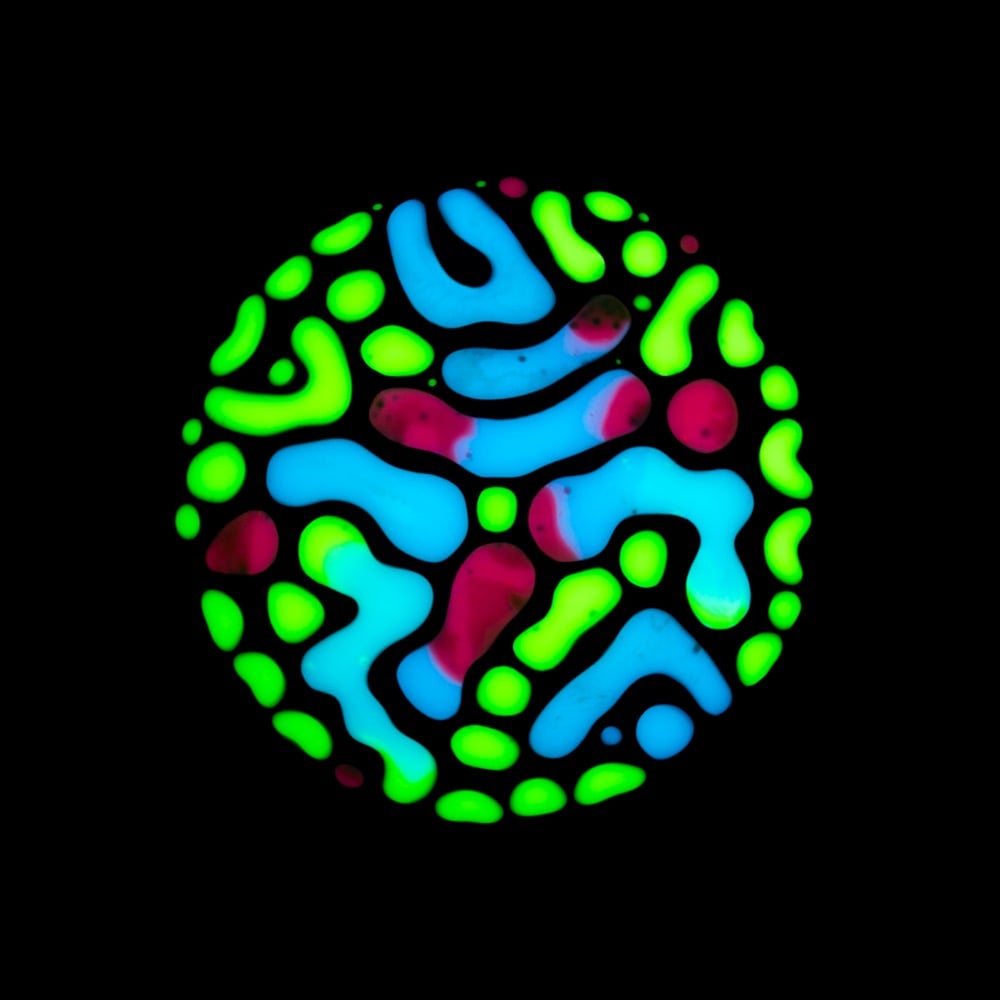
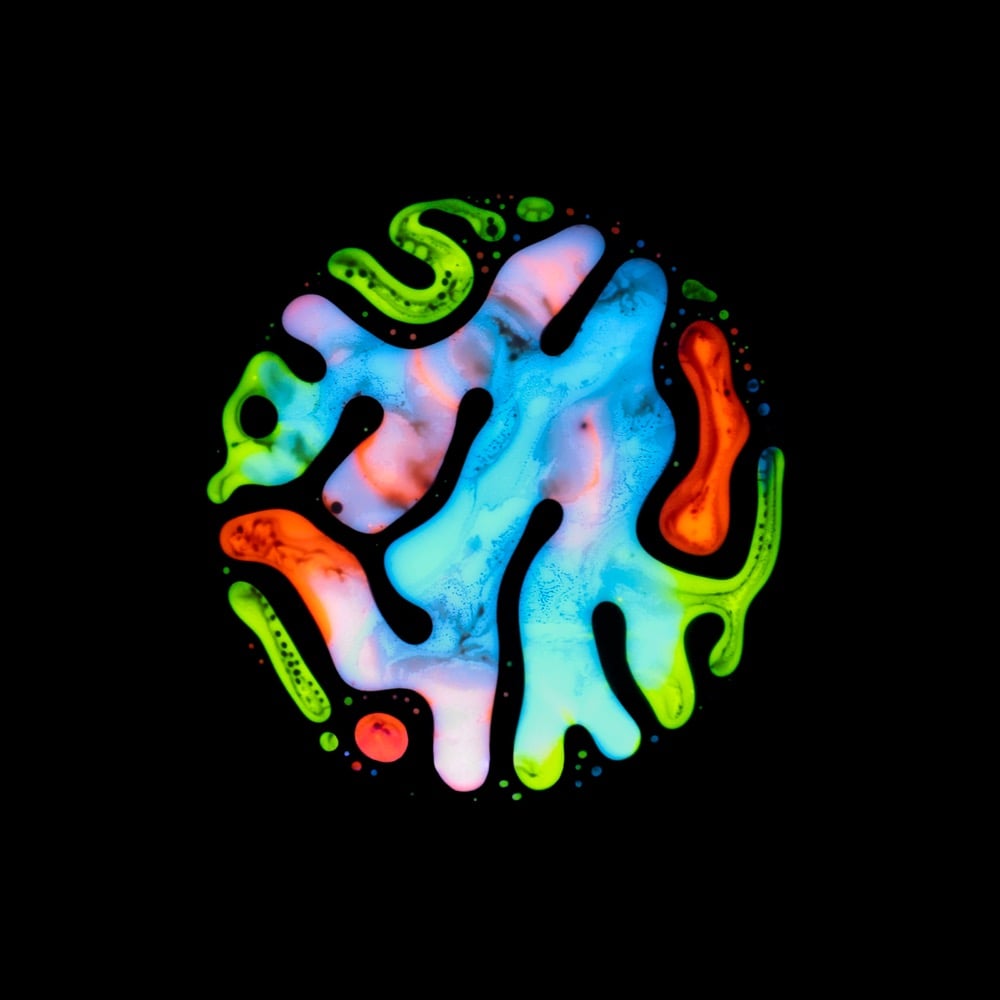
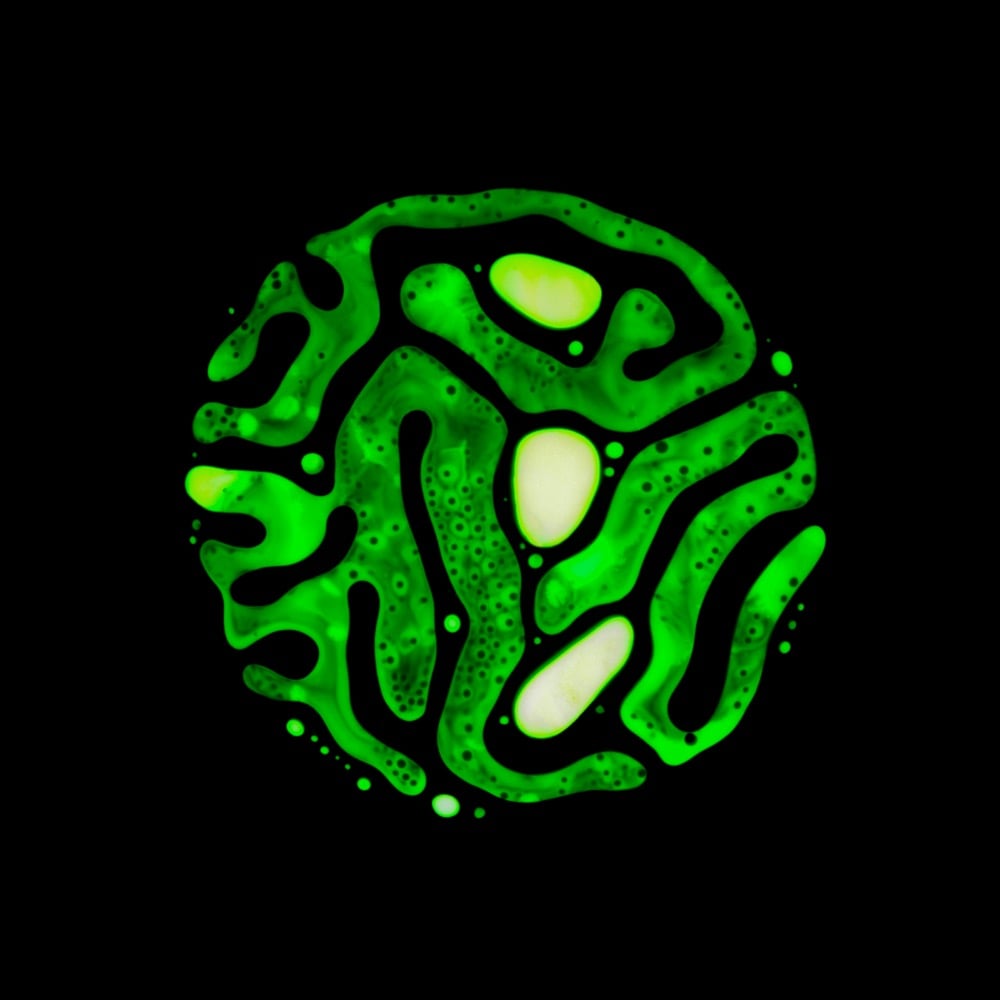

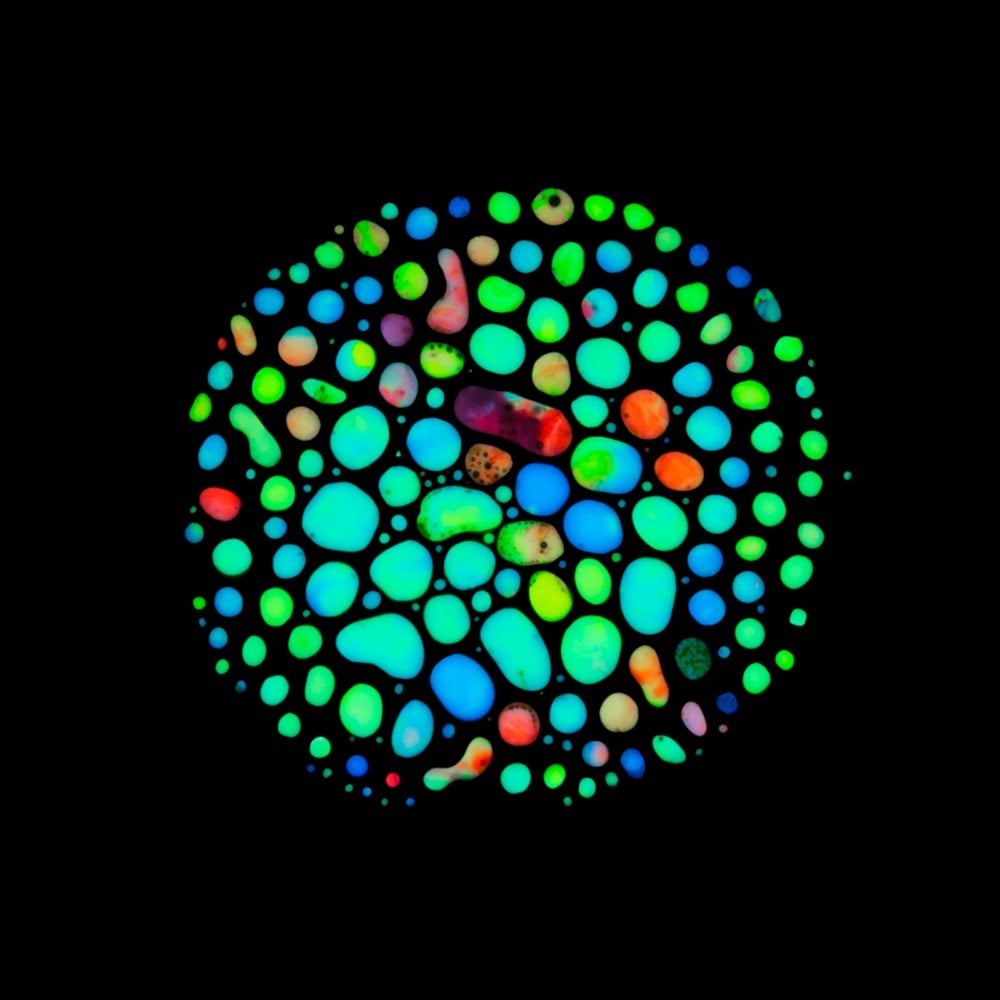
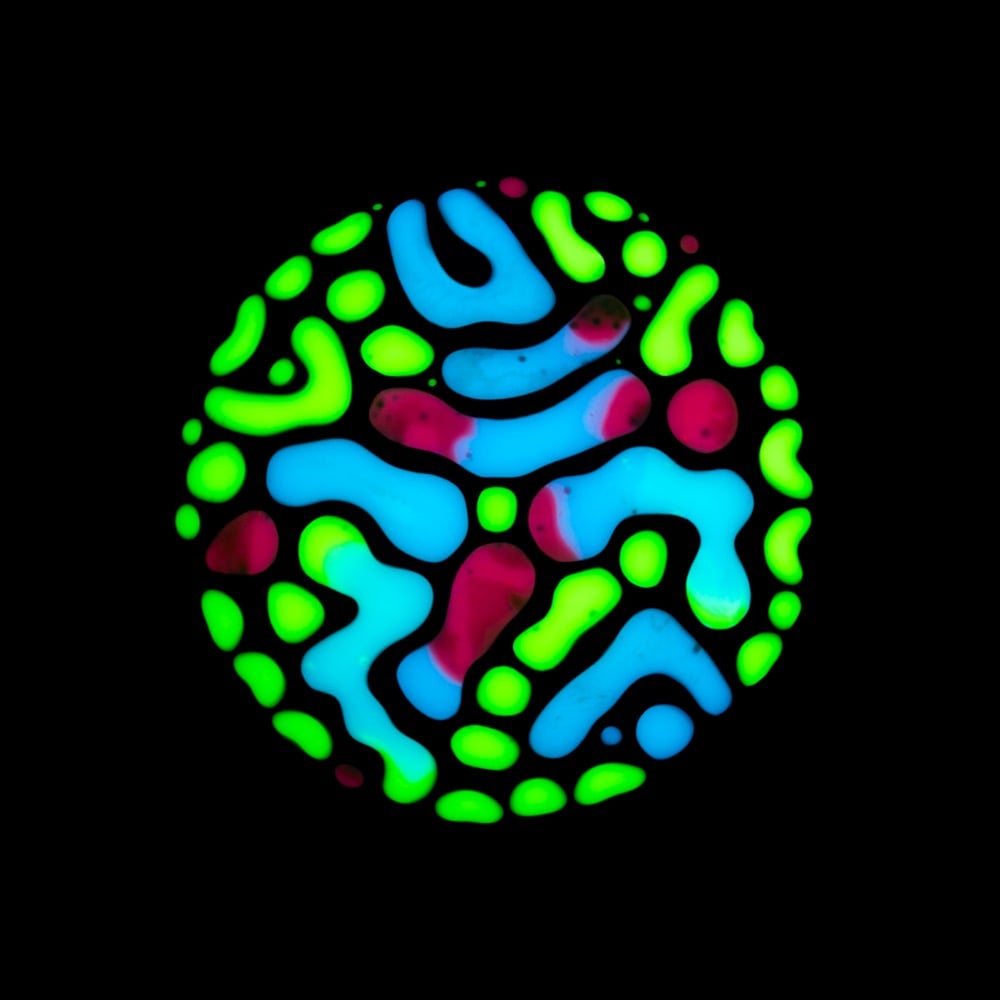
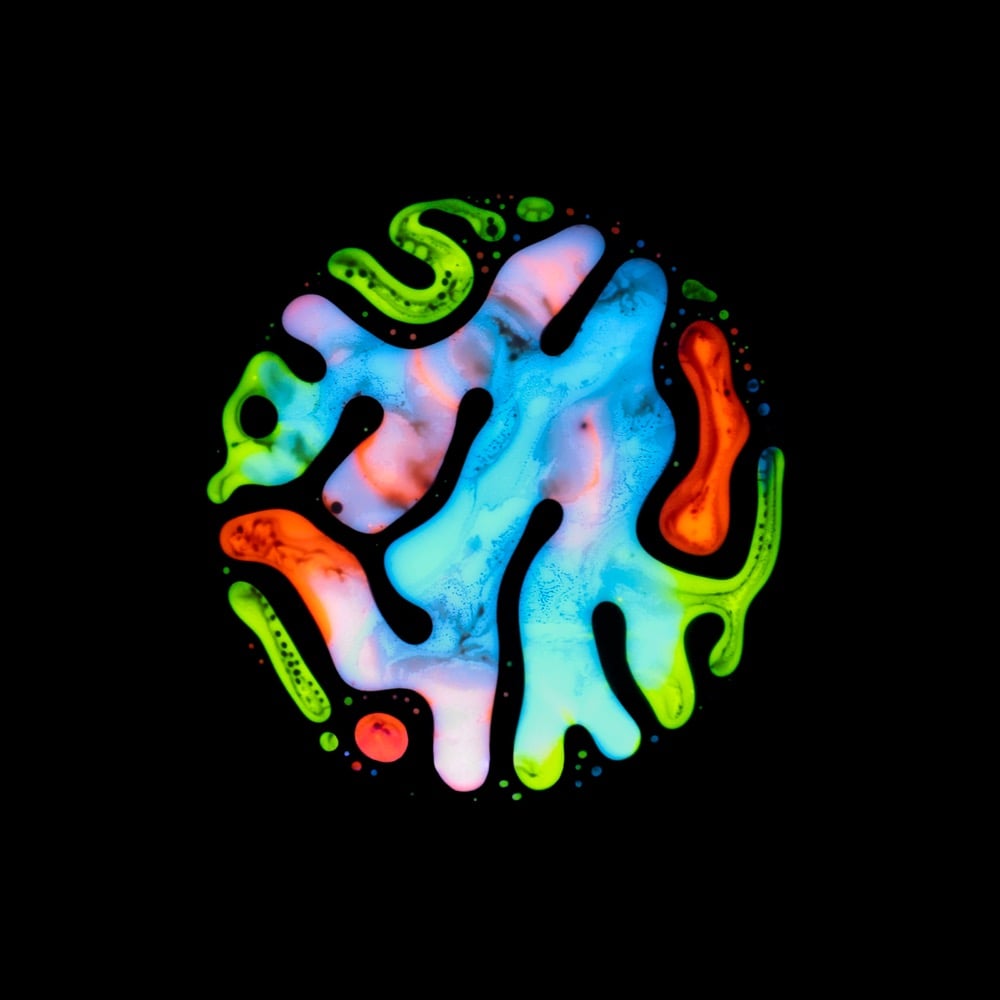
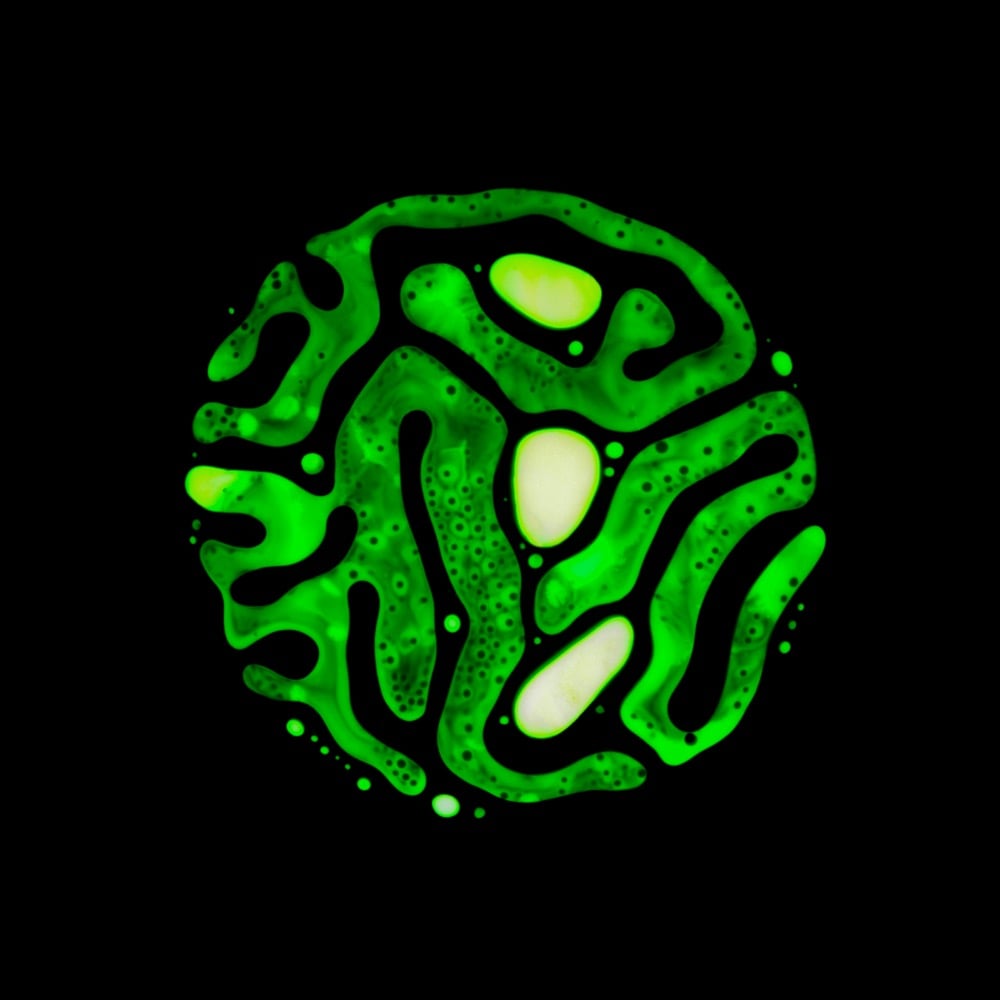
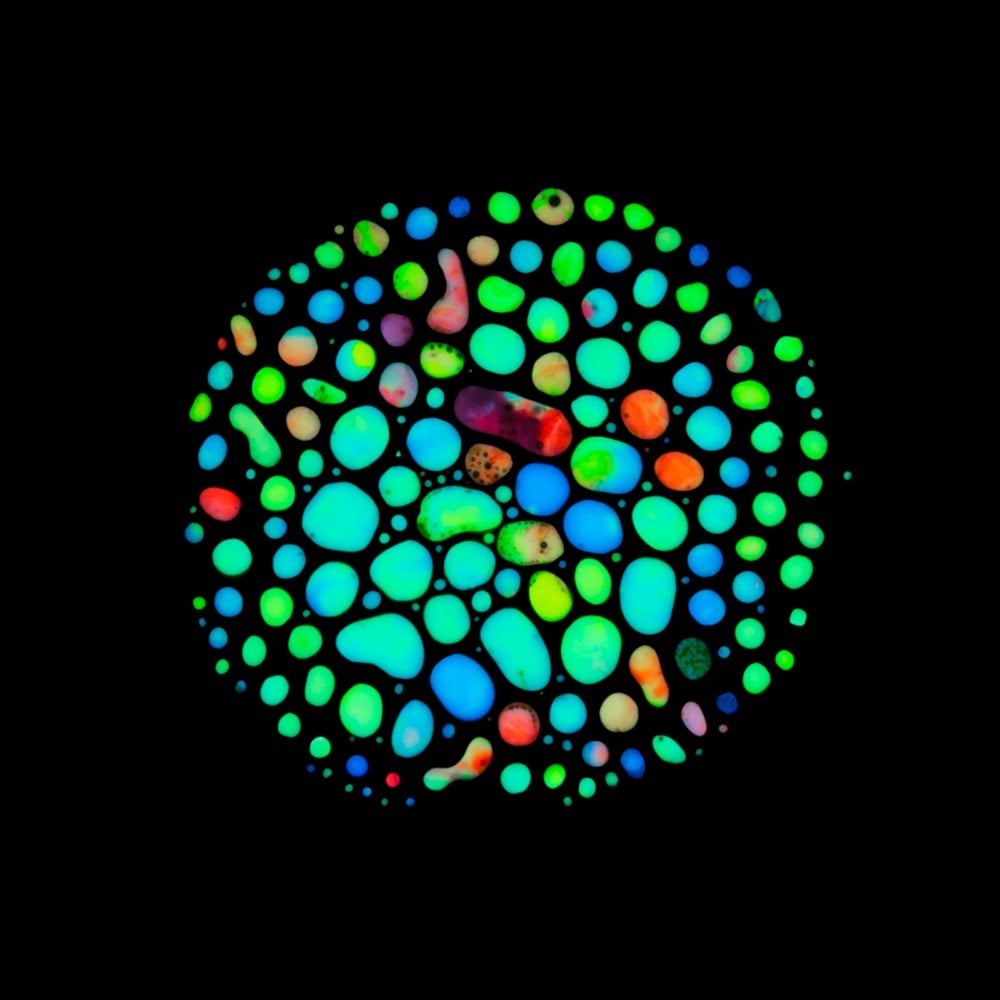
During the course of battling salivary gland tumors over many years, photographer and artist Rubén Álvarez discovered hematopoiesis (the process by which blood cells & blood plasma are formed in the body) as a possible treatment option. The treatment didn’t end up being applicable to his situation, but the process became the inspiration for a very personal project called Haematopoiesis.
This project was inspired by my very personal experiences so I discovered the Hematopoiesis process, while I was looking for treatments for more than 15 pleomorphic adenomas that were located around my head and neck. I went through several surgeries to remove them and reconstruct my facial nerve, as well as almost thirty radiotherapy sessions to prevent these adenomas to appear again.
Álvarez used paint, ferrofluid, and magnets to produce his interpretation of the actual hematopoiesis process. (via moss & fog)
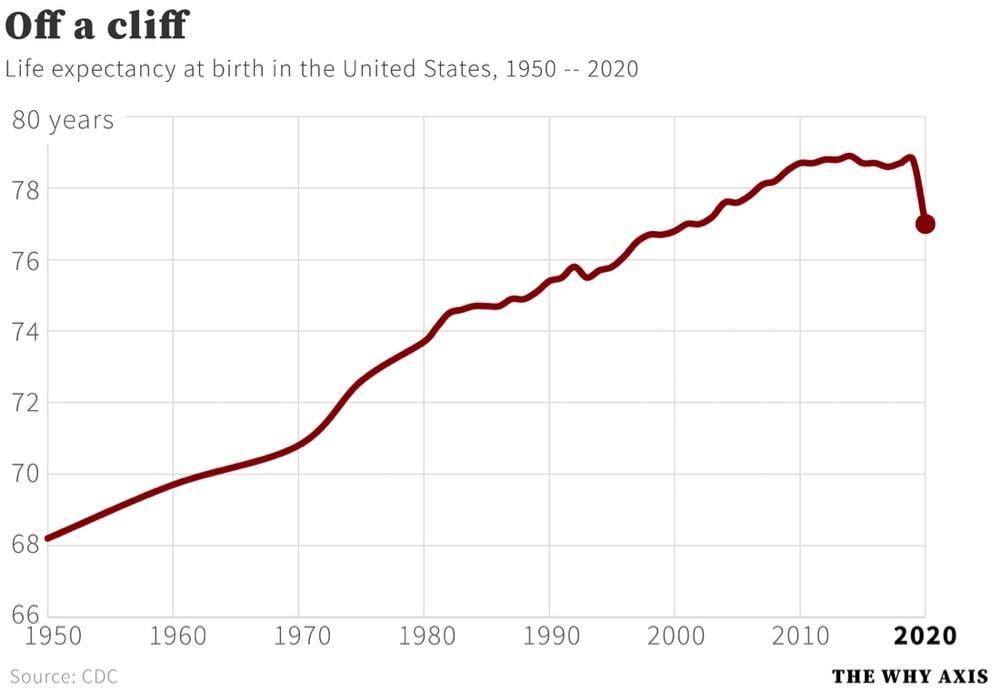
The CDC recently released their report on Mortality in the United States, 2020 and this graph of US life expectancy at birth since 1950 by Christopher Ingraham dramatically summarizes the report’s main finding:
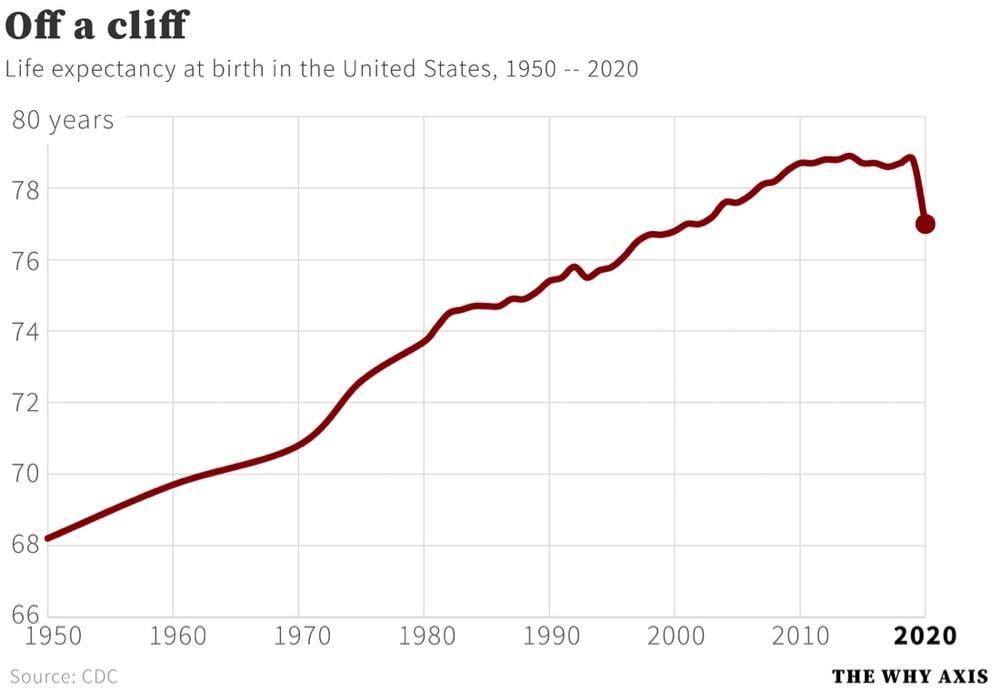
That’s a decrease in life expectancy of 1.8 years from 2019. Here are some more of the report’s significant findings:
In 2020, life expectancy at birth was 77.0 years for the total U.S. population — a decrease of 1.8 years from 78.8 years in 2019. For males, life expectancy decreased 2.1 years from 76.3 in 2019 to 74.2 in 2020. For females, life expectancy decreased 1.5 years from 81.4 in 2019 to 79.9 in 2020.
In 2020, the difference in life expectancy between females and males was 5.7 years, an increase of 0.6 year from 2019.
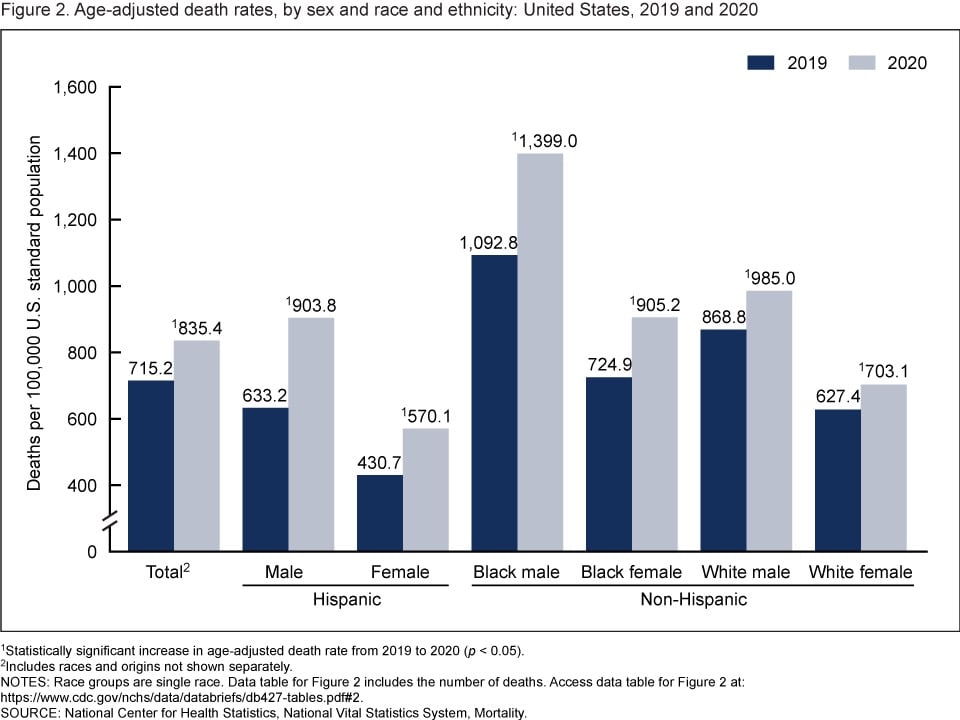
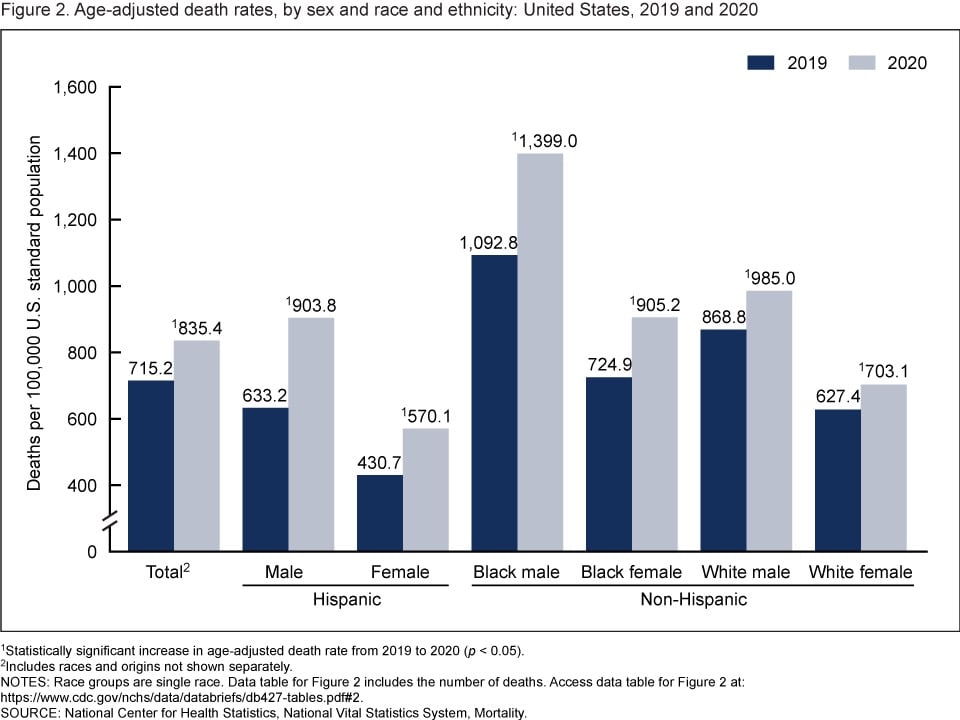
The age-adjusted death rate for the total population increased 16.8% from 715.2 per 100,000 standard population in 2019 to 835.4 in 2020. Age-adjusted death rates increased in 2020 from 2019 for all race-ethnicity-sex groups, increasing 42.7% for Hispanic males, 32.4% for Hispanic females, 28.0% for non-Hispanic Black males, 24.9% for non-Hispanic Black females, 13.4% for non-Hispanic White males, and 12.1% for non-Hispanic White females.
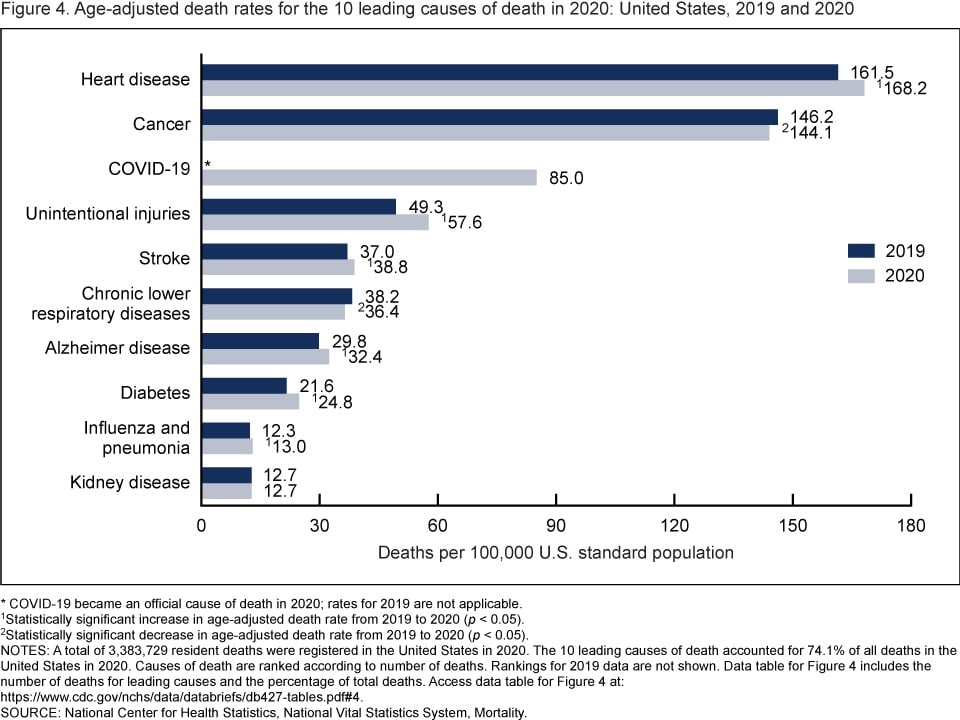
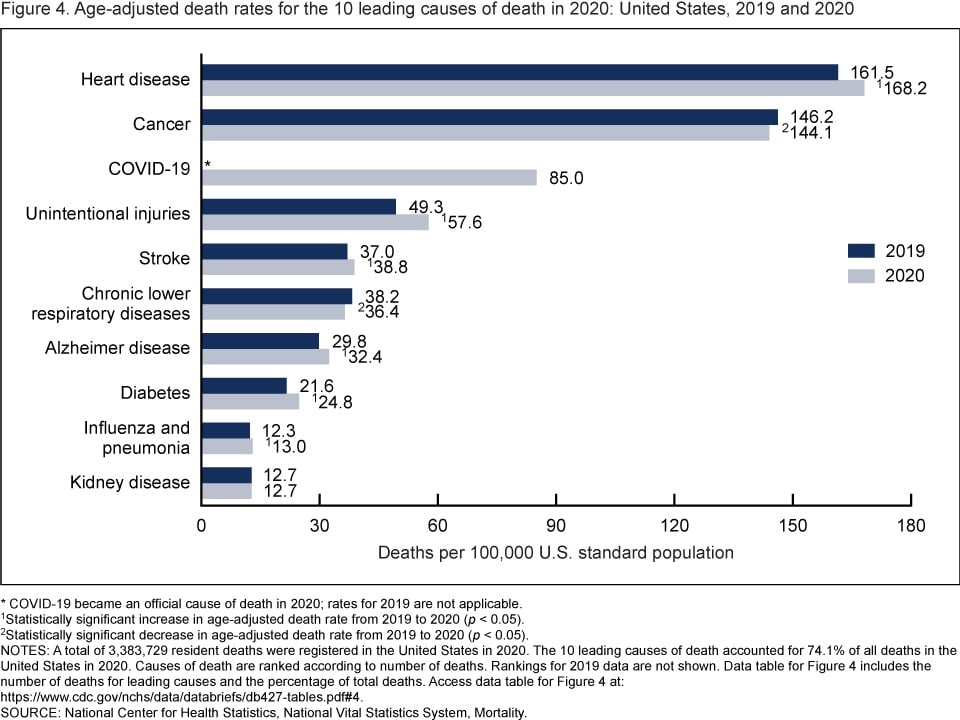
In 2020, 9 of the 10 leading causes of death remained the same as in 2019. The top leading cause was heart disease, followed by cancer. COVID-19, newly added as a cause of death in 2020, became the 3rd leading cause of death. Of the remaining leading causes in 2020 (unintentional injuries, stroke, chronic lower respiratory diseases, Alzheimer disease, diabetes, influenza and pneumonia, and kidney disease), 5 causes changed ranks from 2019. Unintentional injuries, the 3rd leading cause in 2019, became the 4th leading cause in 2020. Chronic lower respiratory diseases, the 4th leading cause in 2019, became the 6th. Alzheimer disease, the 6th leading cause in 2019, became the 7th. Diabetes, the 7th leading cause in 2019, became the 8th. Kidney disease, the 8th leading cause in 2019, became the 10th leading cause in 2020. Stroke, and influenza and pneumonia, remained the 5th and 9th leading causes, respectively. Suicide dropped from the list of 10 leading causes in 2020.
And from the report’s summary:
From 2019 to 2020, the age-adjusted death rate for the total population increased 16.8%. This single-year increase is the largest since the first year that annual mortality data for the entire United States became available. The decrease in life expectancy for the total population of 1.8 years from 2019 to 2020 is the largest single-year decrease in more than 75 years.
Since more people in the US died of Covid in 2021 than in 2020, I’d expect the decline life expectancy and the rise in death rate to continue.
This piece, from Ed Yong, is not at all surprising: America Is Not Ready for Omicron.
America was not prepared for COVID-19 when it arrived. It was not prepared for last winter’s surge. It was not prepared for Delta’s arrival in the summer or its current winter assault. More than 1,000 Americans are still dying of COVID every day, and more have died this year than last. Hospitalizations are rising in 42 states. The University of Nebraska Medical Center in Omaha, which entered the pandemic as arguably the best-prepared hospital in the country, recently went from 70 COVID patients to 110 in four days, leaving its staff “grasping for resolve,” the virologist John Lowe told me. And now comes Omicron.
Will the new and rapidly spreading variant overwhelm the U.S. health-care system? The question is moot because the system is already overwhelmed, in a way that is affecting all patients, COVID or otherwise. “The level of care that we’ve come to expect in our hospitals no longer exists,” Lowe said.
The real unknown is what an Omicron cross will do when it follows a Delta hook. Given what scientists have learned in the three weeks since Omicron’s discovery, “some of the absolute worst-case scenarios that were possible when we saw its genome are off the table, but so are some of the most hopeful scenarios,” Dylan Morris, an evolutionary biologist at UCLA, told me. In any case, America is not prepared for Omicron. The variant’s threat is far greater at the societal level than at the personal one, and policy makers have already cut themselves off from the tools needed to protect the populations they serve. Like the variants that preceded it, Omicron requires individuals to think and act for the collective good — which is to say, it poses a heightened version of the same challenge that the U.S. has failed for two straight years, in bipartisan fashion.
The main point:
Here, then, is the problem: People who are unlikely to be hospitalized by Omicron might still feel reasonably protected, but they can spread the virus to those who are more vulnerable, quickly enough to seriously batter an already collapsing health-care system that will then struggle to care for anyone — vaccinated, boosted, or otherwise. The collective threat is substantially greater than the individual one. And the U.S. is ill-poised to meet it.
Also from Yong: he recently cancelled his 40th birthday party because of Omicron and wrote about how he thought through the decision.
If someone got sick, I know others could too. A week later, many of my friends will spend Christmas with their own families. At best, a cluster of infections at the birthday party would derail those plans, creating days of anxious quarantine or isolation, and forcing the people I love to spend time away from their loved ones. At worst, people might unknowingly carry the virus to their respective families, which might include elderly, immunocompromised, unvaccinated, partially vaccinated, or otherwise vulnerable people. Being born eight days before Christmas creates almost the perfect conditions for one potential super-spreader event to set off many more.
As has been the case the entire pandemic, our political and public health systems are not equipped to collectively combat this virus, so it falls to individuals to make good choices for our communities. It’s a nearly impossible thing to ask to pandemic-weary folks to focus in again on making good personal choices and even harder to achieve if few are willing to do it, but goddammit we have to try.
Last week, a worrisome variant of SARS-CoV-2 burst into the public consciousness: the Omicron variant. The concern among scientists and the public at large is substantial, but it is unfortunately going to take a few weeks to figure out whether those concerns are warranted. For a measured take on what we know now and what we can expect, read these two posts by epidemiologist Dr. Katelyn Jetelina (as well as this one on vaccines).
B.1.1.529 has 32 mutations on the spike protein alone. This is an insane amount of change. As a comparison, Delta had 9 changes on the spike protein. We know that B.1.1.529 is not a “Delta plus” variant. The figure below shows a really long line, with no previous Delta ancestors. So this likely means it mutated over time in one, likely immunocompromised, individual.
Of these, some mutations have properties to escape antibody protection (i.e. outsmart our vaccines and vaccine-induced immunity). There are several mutations association with increased transmissibility. There is a mutation associated with increased infectivity.
That sounds bad but again, we presently do not have enough information to know for sure about any of this. As Jetelina concludes in one of the posts:
We still have more questions than answers. But we will get them soon. Do not take Omicron lightly, but don’t abandon hope either. Our immune systems are incredible.
None of this changes what you can to do right now: Ventilate spaces. Use masks. Test if you have symptoms. Isolate if positive. Get vaccinated. Get boosted.
This Science piece by Kai Kupferschmidt also provides a great overview about where we’re at with Omicron, without the sensationalism.
Whether or not Omicron turns out to be another pandemic gamechanger, the lesson we should take from it (but probably won’t) is that grave danger is lurking in that virus and we need to get *everyone* *everywhere* vaccinated, we need free and ubiquitous rapid testing *everywhere*, we need to focus on indoor ventilation, we need to continue to use measures like distancing and mask-wearing, and we need to keep doing all of the other things in the Swiss cheese model of pandemic defense. Anything else is just continuing our idiotic streak with this virus of fucking around and then finding out. (via jodi ettenberg & eric topol)
In the United States and in many other countries around the world, we’re slowly shifting away from the Covid-19 pandemic to SARS-CoV-2 being endemic (like the flu), Dr. Lucy McBride argues that we need to recalibrate our risk calculations and expectations of what’s safe & dangerous. From A COVID Serenity Prayer in The Atlantic:
For the past 18 months, my patients have craved straightforward answers: a simple “Yes-it’s perfectly safe” or “Go for it. Have fun!” or even a “No, you absolutely cannot” to quiet the endless loops of risk calculations. But medicine is not about certainty. It never has been.
The two things that patients want-reassurance that they won’t get COVID-19 and permission to engage in life-I cannot deliver, and I never will be able to. SARS-CoV-2 is here to stay. The virus will be woven into our everyday existence much like RSV, influenza, and other common coronaviruses are. The question isn’t whether we’ll be exposed to the novel coronavirus; it’s when.
And although many of us will inevitably get COVID-19, for the majority of vaccinated people, it won’t be so bad. The vaccines weren’t designed to wholly prevent COVID-19; they transformed it into a manageable illness like the flu.
That means that, from a decision-making perspective, we’re starting to reach the acceptance phase of the pandemic: a time when we must recalibrate our individual risk gauges, which have been completely thrown out of whack. The approach I’m embracing with patients boils down to a secular version of the serenity prayer. We need “the serenity to accept the things [we] cannot change, courage to change the things [we] can, and the wisdom to know the difference.”
Within the past 50 years, the global community has solved two huge problems that had the potential to harm every person on Earth. Smallpox once killed 30% of the people who contracted the disease but through the invention of an effective, safe vaccine and an intense effort that began in the 1960s, smallpox was completely eradicated by 1980. In the 1980s, scientists discovered a hole in the ozone layer that protects the Earth from UV radiation; further depletion would have caused major problems with the world’s food supply and an epidemic of skin cancer. Forty years later, we’ve virtually eliminated the chemicals causing the depletion and ozone losses have stabilized and have recently shown improvement.
So how did we do it? The short video above talks through each of challenges, how they were met (science + politics + a bit of luck), and how we might apply these lessons to the big problems of today (climate emergency, the pandemic).
Dr. Alan Braid, a practicing OB/GYN in the state of Texas for 45 years, explains why he provided medical care in the form of an abortion to a woman in violation of the state’s absurd and dangerous new law.
A new Texas law, known as S.B. 8, virtually banned any abortion beyond about the sixth week of pregnancy. It shut down about 80 percent of the abortion services we provide. Anyone who suspects I have violated the new law can sue me for at least $10,000. They could also sue anybody who helps a person obtain an abortion past the new limit, including, apparently, the driver who brings a patient to my clinic.
For me, it is 1972 all over again.
And that is why, on the morning of Sept. 6, I provided an abortion to a woman who, though still in her first trimester, was beyond the state’s new limit. I acted because I had a duty of care to this patient, as I do for all patients, and because she has a fundamental right to receive this care.
I fully understood that there could be legal consequences — but I wanted to make sure that Texas didn’t get away with its bid to prevent this blatantly unconstitutional law from being tested.
Braid concluded his piece: “I believe abortion is an essential part of health care.” Absolutely.
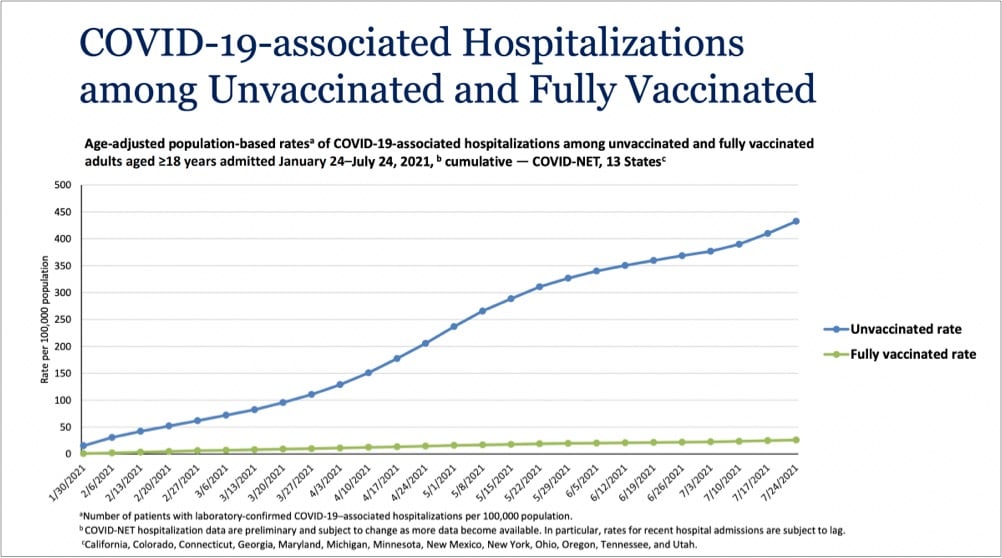
It may seem like sometimes that with the pandemic, we’re back to square one. With the much more contagious Delta variant in play and an increasing number of breakthrough infections, the efficacy of these vaccines that we thought were amazing maybe aren’t? (Or maybe we just need to readjust our expectations?) But in terms of what these vaccines were specifically developed for — reducing & preventing severe disease and death — they are still very much doing their job. Just take a look at this graph from a White House Covid-19 press briefing yesterday:
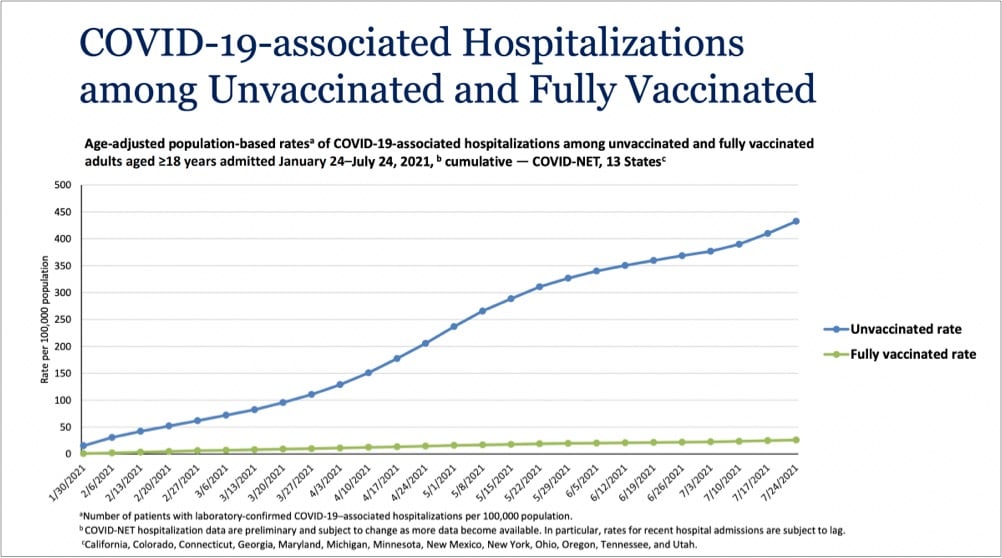
Even with Delta endemic in the country, the vaccines are providing extraordinary protection against infections severe enough to land folks in the hospital. In a recent CDC study of infections and hospitalizations in Los Angeles County, they report that on July 25, the hospitalization rate of unvaccinated people was 29.2 times that of fully vaccinated persons. 29 times the protection is astounding for a medical intervention. These vaccines work, we’re lucky to have them, and we need to get as many people worldwide as we can vaccinated as quickly as we can. Period.
You might want to take a deep breath or do a couple of laps around the house before watching this video about a community in the Ozarks with a very low Covid-19 vaccination rate. Here’s a sample. An ICU patient wearing an oxygen mask on why he didn’t get vaccinated:
I’m more of a libertarian and I don’t like being told what I have to do. I’m still not completely 100% sold on the inoculation.
Video narrator:
It was eerie to hear Christopher insist on his individual freedoms even as he struggled to breathe.
Can you hear me screaming all the way from my desk to wherever you are? I don’t like being told what I have to do?! Fucking hell. And this:
There’s no better place to see the impact of this political rhetoric than in the hospital. Only about 50 percent of the staff are vaccinated. None of the unvaccinated staffers were willing to talk.
Absolutely maddening. I want off this ride.
For The Atlantic, Katherine Wu writes about the difficulty of communicating how vaccines work and how they protect individuals and communities from disease: Vaccines Are Like Sunscreen… No, Wait, Airbags… No, Wait…
Unfortunately, communal benefit is harder to define, harder to quantify, and harder to describe than individual protection, because “it’s not the way Americans are used to thinking about things,” Neil Lewis, a behavioral scientist and communications expert at Cornell, told me. That’s in part because communal risk isn’t characteristic of the health perils people in wealthy countries are accustomed to facing: heart disease, stroke, diabetes, cancer. Maybe that’s part of why we gravitate toward individual-focused comparisons. Slipping into a pandemic-compatible, population-based frame of mind is a big shift. In the age of COVID-19, “there’s been a lot of focus on the individual,” Lewis told me. That’s pretty at odds “with how infection works.”
As someone who has struggled with analogizing the virus & vaccines, I was nodding my head a lot while reading this. Something I’ve noticed in recent years that Wu didn’t get into is that readers desire precision in metaphors and analogies, even though metaphor is — by definition! — not supposed to be taken literally. People seem much more interested in taking analogies apart, identifying what doesn’t work, and discarding them rather than — more generously and constructively IMO — using them as the author intended to better understand the subject matter. The perfect metaphor doesn’t exist because then it wouldn’t be a metaphor.
I’m just going to go ahead and say it right up front here: if you had certain expectations in May/June about how the pandemic was going to end in the US (or was even thinking it was over), you need to throw much of that mindset in the trash and start again because the Delta variant of SARS-CoV-2 has changed the game. I know this sucks to hear,1 but Delta is sufficiently different that we need to reset and stop assuming we can solely rely on the vaccines to stop Covid-19 from spreading. Ed Yong’s typically excellent piece on how delta has changed the pandemic’s endgame is helping me wrap my head around this.
But something is different now — the virus. “The models in late spring were pretty consistent that we were going to have a ‘normal’ summer,” Samuel Scarpino of the Rockefeller Foundation, who studies infectious-disease dynamics, told me. “Obviously, that’s not where we are.” In part, he says, people underestimated how transmissible Delta is, or what that would mean. The original SARS-CoV-2 virus had a basic reproduction number, or R0, of 2 to 3, meaning that each infected person spreads it to two or three people. Those are average figures: In practice, the virus spread in uneven bursts, with relatively few people infecting large clusters in super-spreading events. But the CDC estimates that Delta’s R0 lies between 5 and 9, which “is shockingly high,” Eleanor Murray, an epidemiologist at Boston University, told me. At that level, “its reliance on super-spreading events basically goes away,” Scarpino said.
In simple terms, many people who caught the original virus didn’t pass it to anyone, but most people who catch Delta create clusters of infection. That partly explains why cases have risen so explosively. It also means that the virus will almost certainly be a permanent part of our lives, even as vaccines blunt its ability to cause death and severe disease.
And a reminder, as we “argue over small measures” here in the US, that most of the world is in a much worse place:
Pandemics end. But this one is not yet over, and especially not globally. Just 16 percent of the world’s population is fully vaccinated. Many countries, where barely 1 percent of people have received a single dose, are “in for a tough year of either lockdowns or catastrophic epidemics,” Adam Kucharski, the infectious-disease modeler, told me. The U.S. and the U.K. are further along the path to endemicity, “but they’re not there yet, and that last slog is often the toughest,” he added. “I have limited sympathy for people who are arguing over small measures in rich countries when we have uncontrolled epidemics in large parts of the world.”
Where I think Yong’s piece stumbles a little is in its emphasis of the current vaccines’ protection against infection from Delta. As David Wallace-Wells explains in his piece Don’t Panic, But Breakthrough Cases May Be a Bigger Problem Than You’ve Been Told, vaccines still offer excellent protection against severe infection, hospitalization, and death, but there is evidence that breakthrough infections are more common than many public health officials are saying. The problem lies with the use of statistics from before vaccines and Delta were prevalent:
Almost all of these calculations about the share of breakthrough cases have been made using year-to-date 2021 data, which include several months before mass vaccination (when by definition vanishingly few breakthrough cases could have occurred) during which time the vast majority of the year’s total cases and deaths took place (during the winter surge). This is a corollary to the reassuring principle you might’ve heard, over the last few weeks, that as vaccination levels grow we would expect the percentage of vaccinated cases will, too — the implication being that we shouldn’t worry too much over panicked headlines about the relative share of vaccinated cases in a state or ICU but instead focus on the absolute number of those cases in making a judgment about vaccine protection across a population. This is true. But it also means that when vaccination levels were very low, there were inevitably very few breakthrough cases, too. That means that to calculate a prevalence ratio for cases or deaths using the full year’s data requires you to effectively divide a numerator of four months of data by a denominator of seven months of data. And because those first few brutal months of the year were exceptional ones that do not reflect anything like the present state of vaccination or the disease, they throw off the ratios even further. Two-thirds of 2021 cases and 80 percent of deaths came before April 1, when only 15 percent of the country was fully vaccinated, which means calculating year-to-date ratios means possibly underestimating the prevalence of breakthrough cases by a factor of three and breakthrough deaths by a factor of five. And if the ratios are calculated using data sets that end before the Delta surge, as many have been, that adds an additional distortion, since both breakthrough cases and severe illness among the vaccinated appear to be significantly more common with this variant than with previous ones.
Vaccines are still the best way to protect yourself and your community from Covid-19. The vaccines are still really good, better than we could have hoped for. But they’re not magic and with the rise of Delta (and potentially worse variants on the horizon if the virus is allowed to continue to spread unchecked and mutate), we need to keep doing the other things (masking, distancing, ventilation, etc.) in order to keep the virus in check and avoid lockdowns, school closings, outbreaks, and mass death. We’ve got the tools; we just need to summon the will and be in the right mindset.
The Panola Project is a short film by Rachael DeCruz and Jeremy Levine that follows the efforts of local convenience store owner Dorothy Oliver to get the people in her small Alabama community vaccinated against Covid-19. A trusted member of her community, Oliver teams up with county commissioner Drucilla Russ-Jackson to call & go door-to-door, talking with people one-on-one, cajoling and telling personal stories of loss to get folks signed up for a mobile vaccination clinic.
In the film, Oliver and Russ-Jackson arrange for a hospital to set up a pop-up site in Panola, but the site will only be established if they get at least forty people to sign up to take the vaccine. We follow Oliver as she goes door to door, talking people into signing up, lightly cajoling them about their fears and concerns. When I asked her how she does it, her answer was disarmingly simple: “I just be nice to them,” she said. “I don’t go at them saying, ‘You gotta do that.’” DeCruz, too, was struck by the way Oliver and Jackson talked to people who were on the fence about the vaccine, an issue more often discussed with stridency of various types. “There’s this very warm and kind of loving and caring way that Dorothy and Ms. Jackson approached those conversations, even when people aren’t in agreement. And it wasn’t done in a way that’s, like, ‘I know better than you.’ “
Oliver’s charm with the skeptics is remarkable, but so is her determination to bring the vaccine to her underserved town. Most of the women and men Oliver talked to leaped at the opportunity to sign up for the vaccine. On vaccine day, they rolled down their car windows to thank her. “We appreciate y’all giving it to us, because a lot of people don’t really know where to go to take these vaccines,” one woman tells her. Vaccine hesitancy in Black communities has been harped on in the media, but those conversations can gloss over questions of availability. Levine told me that they were struck by how many people had put off vaccination for logistical rather than ideological reasons. In Panola, he says, they regularly heard people say, “I want the shot. How do I get this? I don’t have a car; how am I going to get forty miles to the closest hospital and back?”
The result? In a state with one of the lowest vaccination rates in the country, 94% of adults in Panola have been vaccinated, due in part to Oliver’s and Russ-Jackson’s efforts.
This piece by Susan Matthews is really helpful for those of us who are vaccinated and trying to figure out what their risks are regarding the much more transmissible delta variant of SARS-CoV-2. Covid-19 is endemic now — how do we live with that? What reasonable actions should we take to keep ourselves, our communities, and our loved ones safe?
All of this is making people — yes, probably mostly vaccinated people — rethink the basic questions they thought their vaccine had answered for them: Can I go to restaurants and bars unmasked? Can I go back to the office? Can I see my grandma? Can I go on vacation? Can I unmask at my people-facing job? Can I have a wedding, or a party? The answer to those questions is not quite as easy as “yes, if you’re vaccinated.” It depends partly on how many in your group are vaccinated, but the actual answer is basically the same as it’s been all pandemic: It depends on your risk tolerance, it depends on what is happening with case counts locally (though, as more people travel, this might become a less reliable tool), and it depends on any unique risk factors in your group. Kass’ perspective felt novel to me: She said she suspects that in the end, a lot of people are going to end up boosting their immunity by suffering through a mild case of COVID. So no one should feel that bad about getting sick after they’re vaxxed. What matters is getting the order right: “If everyone who gets vaccinated still gets COVID but doesn’t die, that’s a success,” she said. The issue is that it doesn’t feel like a success for vaccinated people. Plus, “if you get infected after you’re vaxxed, it’s all you talk about,” she said. And right now, that’s understandably freaking out a lot of vaccinated people who thought they were in the clear.
Long Covid isn’t mentioned anywhere in here though — surely that has to be part of the conversation here (although anecdotally it doesn’t seem like too much of a worry).
Dr. Brytney Cobia treats Covid-19 patients at the Grandview Medical Center in Birmingham, Alabama, a state that ranks last in the US in fully vaccinated adults. In a recent Facebook post, Cobia shares that people are willing to get vaccinated after having to watch an unvaccinated member of their family die from Covid.
I’ve made a LOT of progress encouraging people to get vaccinated lately!!! Do you want to know how? I’m admitting young healthy people to the hospital with very serious COVID infections. One of the last things they do before they’re intubated is beg me for the vaccine. I hold their hand and tell them that I’m sorry, but it’s too late. A few days later when I call time of death, I hug their family members and I tell them the best way to honor their loved one is to go get vaccinated and encourage everyone they know to do the same. They cry. And they tell me they didn’t know. They thought it was a hoax. They thought it was political. They thought because they had a certain blood type or a certain skin color they wouldn’t get as sick. They thought it was ‘just the flu’. But they were wrong. And they wish they could go back. But they can’t. So they thank me and they go get the vaccine. And I go back to my office, write their death note, and say a small prayer that this loss will save more lives.
Heartbreaking.
Olga Khazan writing for The Atlantic:
After an inept coronavirus response, will the United States do better when the next pandemic strikes? Experts generally agree that America learned from the past year, and that the next public-health crisis won’t be quite as bewildering. But America’s pandemic preparedness still has major gaps, some of which are too big for any one administration to fix. In recent weeks, I’ve called back many of the experts I interviewed over the past 18 months about masks, testing, contact tracing, quarantine, and more. I asked them, “Are we ready for another one?” The short answer is “Not quite.” The long answer is that being truly “ready” will be harder than anyone realizes.
The Trump administration mishandled the American response to Covid-19 so completely that it’s tempting to pin most of the pandemic carnage on him. But the more I read about the pandemic (Michael Lewis’s The Premonition is a recent example), the more I have come to believe that the majority of the American pandemic deaths were baked in, no matter who was President. Trump was definitely a worst-case scenario, but even a more competent person in the White House in Jan 2020 (like Clinton or Sanders or Romney) would not have done so much better. Poor public health infrastructure, politicized government agencies, no mandatory paid leave, an overpriced healthcare system that only works for some, uncoordinated national response (+ federalism), years of defunding government programs, a reactive (rather than proactive) CDC, unhealthy populace, poverty, systemic racism in medicine, entitled individualism, high rate of uninsured people, growing anti-science sentiment — the pandemic was destined to race through the United States like a brush fire no matter what.
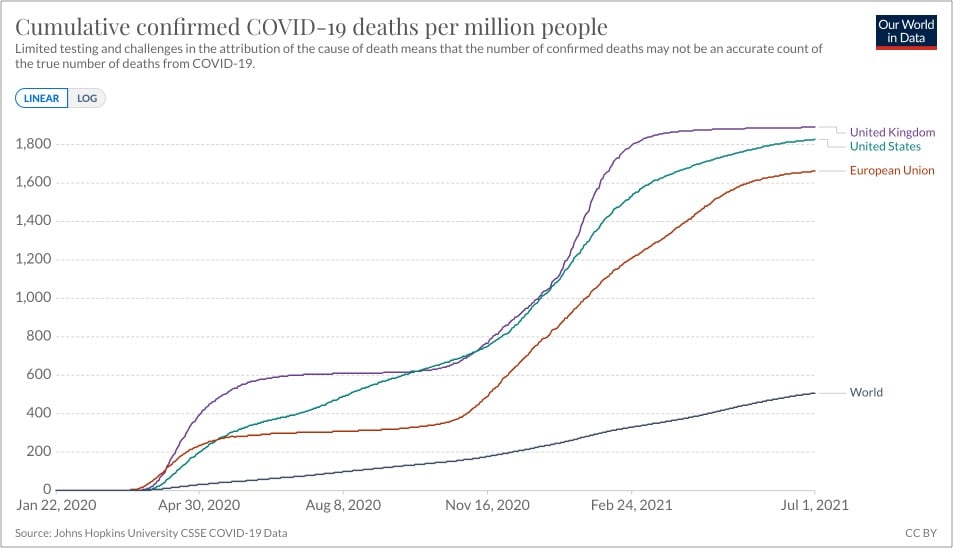
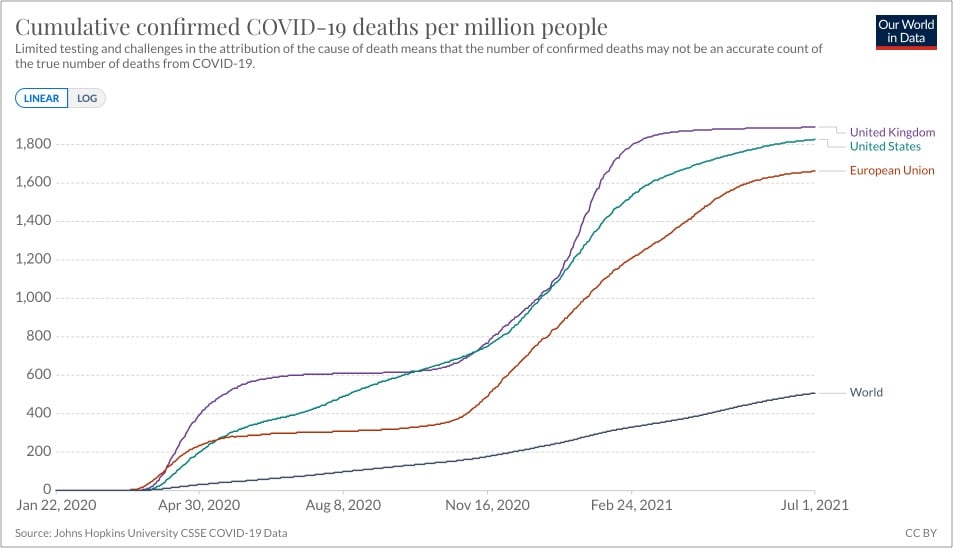
Even the European Union, whose member nations do not share many of America’s aforementioned challenges (but have other issues), did only marginally better than the US in preventing Covid deaths. The UK did worse:
Over the past several months, I’ve read several pieces about the possible origins of SARS-CoV-2 and have been frustrated with the certainty with which folks who should know better have embraced the “lab leak hypothesis”. So, I was happy to see Zeynep Tufekci’s characteristically even-handed and comprehensive overview of the evidence about the virus’s origins in the NY Times.
While the Chinese government’s obstruction may keep us from knowing for sure whether the virus, SARS-CoV-2, came from the wild directly or through a lab in Wuhan or if genetic experimentation was involved, what we know already is troubling.
Years of research on the dangers of coronaviruses, and the broader history of lab accidents and errors around the world, provided scientists with plenty of reasons to proceed with caution as they investigated this class of pathogens. But troubling safety practices persisted.
Worse, researchers’ success at uncovering new threats did not always translate into preparedness.
Even if the coronavirus jumped from animal to human without the involvement of research activities, the groundwork for a potential disaster had been laid for years, and learning its lessons is essential to preventing others.
Is it possible that SARS-CoV-2 came from a lab? Yes. Is it probable? We can’t know that right now. It’s a tantalizing puzzle involving a possible cover-up, but irresponsibly assigning certainty to the situation does no one but attention-seeking pundits any good.

- You 100% do not want to get Covid-19.
- You are immunocompromised. Millions of people have immune conditions that make contracting Covid-19 much more dangerous for them.
- You’re traumatized from “the mental and emotional toll of the last year”.
- Because you need to be around people you suspect may not be vaccinated or taking Covid-19 seriously (e.g. as part of your job).
- You’re not feeling well and want to make sure to protect others around you.
- Because you want to signal to others that you are being safe and thinking of the health and wellness of those around you.
- You live in a household with unvaccinated people (kids, for example) and want to make sure to protect them.
- Because your personal risk tolerance is lower than other people’s.
- You need some time to feel comfortable enough taking your mask off around others after more than a year of that very behavior being dangerous.
- Because you want to.
- But mostly because it is NONE OF ANYONE’S GODDAMN CONCERN if you choose to keep wearing a mask. Fuck off! Mind your own business!

Urine color is an indicator of how hydrated you are and Pantone are the color experts, so of course they’ve teamed up with a Scottish bottled water company to produce a chart with 5 color gradations that help you determine your hydration level. But 10 glasses of water a day?! I’m not sure the science supports that, particularly since we get a lot of our recommended intake from regular food & beverage consumption.
It remains unclear where the “8 x 8” water intake recommendation comes from. Perhaps, this two-liter intake threshold is derived from a misinterpretation of original recommendations offered by the U.S. Food and Nutrition Board in 1945 as well as the 2017 European Food Safety Authority, which states the daily recommended amount of water includes all beverages plus the moisture contained in foods.
This means that the moisture contained in foods, especially fresh fruits, sodas, juices, soups, milk, coffee and, yes, even beer, contributes to this daily recommended water requirement. These guidelines go on to suggest that most of the recommended water content can be accomplished without drinking additional cups of plain water.
(via print)
In a letter published in The Lancet, a group of scholars argue, with an extensive review of the available evidence, that the primary mode of transmission from human to human of the virus responsible for Covid-19 is via aerosols, not through larger particles called droplets or through fomites (transfer from surfaces). Here are three of their ten reasons why:
Third, asymptomatic or presymptomatic transmission of SARS-CoV-2 from people who are not coughing or sneezing is likely to account for at least a third, and perhaps up to 59%, of all transmission globally and is a key way SARS-CoV-2 has spread around the world, supportive of a predominantly airborne mode of transmission. Direct measurements show that speaking produces thousands of aerosol particles and few large droplets, which supports the airborne route.
Fourth, transmission of SARS-CoV-2 is higher indoors than outdoors and is substantially reduced by indoor ventilation. Both observations support a predominantly airborne route of transmission.
Fifth, nosocomial infections have been documented in health-care organisations, where there have been strict contact-and-droplet precautions and use of personal protective equipment (PPE) designed to protect against droplet but not aerosol exposure.
The letter concludes with a plea by the authors for public health officials to finally embrace this reality: “The public health community should act accordingly and without further delay.”
I can’t believe we’re actually still arguing about this. One of the authors, Jose-Luis Jimenez, wrote this seminal Time magazine piece that provided the smoke analogy that is the mental model I’ve been using to think about potential risks during the pandemic.
When it comes to COVID-19, the evidence overwhelmingly supports aerosol transmission, and there are no strong arguments against it. For example, contact tracing has found that much COVID-19 transmission occurs in close proximity, but that many people who share the same home with an infected person do not get the disease. To understand why, it is useful to use cigarette or vaping smoke (which is also an aerosol) as an analog. Imagine sharing a home with a smoker: if you stood close to the smoker while talking, you would inhale a great deal of smoke. Replace the smoke with virus-containing aerosols, which behave very similarly, and the impact is similar: the closer you are to someone releasing virus-carrying aerosols, the more likely you are to breathe in larger amounts of virus. We know from detailed, rigorous studies that when individuals talk in close proximity, aerosols dominate transmission and droplets are nearly negligible.
Another of the authors, Zeynep Tufekci, has been arguing the case for aerosols (and masks & overdispersion) since early in the pandemic, and she succinctly explained in a Twitter thread how predominantly aerosol transmission fits with the mitigation methods that have really worked around the world:
Airborne transmission unites three things crucial to recognize for effective COVID-19 mitigation: transmission without symptoms (thus aerosols), clusters driving the epidemic (also aerosols) and masks/ventilation indoors being key (hey, also aerosols). This framework is coherent.
Her whole thread is worth a read — like this bit about how other respiratory pathogens are likely spread by aerosols and not droplets (as commonly believed):
Fascinatingly, you search the scientific record high and low, but there really is little to no direct evidence for gravity-sprayed droplets being predominant mode of transmission for respiratory illnesses outside of coughing/sneezing. It’s many… assumptions. Like a tradition.
If any good comes out of the pandemic at all, a better and more useful scientific understanding of how respiratory pathogens are transmitted would be a good start.
Update: One of the authors, Trisha Greenhalgh, responds succinctly to criticisms of the paper in this Twitter thread.
Criticism 1: “The paper is just opinion, and several authors aren’t even doctors.”
Response: No. It’s well-researched scholarly argument, produced by an interdisciplinary team of 6 professors including 3 docs, 2 aerosol scientists and 1 social scientist.
In 1955, epidemiologist Thomas Francis Jr. announced the results of a field trial of the polio vaccine that Jonas Salk had developed. America erupted in joy.
Now a phalanx of bulky television cameras focussed on Francis as he prepared to report on the efficacy of the vaccine. He had good news to share: to cheers from the audience, he explained that the Salk vaccine was sixty to seventy per cent effective against the most prevalent strain of poliovirus, and ninety per cent effective against the other, less common strains. All this had been shown through what was, at that time, the largest vaccine trial ever conducted.
All afternoon and evening, church bells rang out across America. People flooded into the streets, kissing and embracing; parents hugged their kids with joy and relief. Salk became an instant national hero, turning down the offer of a ticker-tape parade in New York City; President Dwight D. Eisenhower invited him to the White House and, later, asked Congress to award him a Congressional Gold Medal. That night, from the kitchen of a colleague’s house, Salk — whose name was being touted in newspapers, magazines, radio reports, and television news broadcasts around the world — gave his first network-TV interview to Edward R. Murrow, whose show “See It Now” had exposed the tactics of Senator Joseph McCarthy a year earlier. Blushing in admiration, Murrow asked the doctor, “Who owns the patent on this vaccine?” “The people,” Salk said, nobly. “There is no patent. Could you patent the sun?”
In the days that followed, schoolchildren were instructed by their teachers to write thank-you notes to Salk. Universities lined up to offer him honorary degrees. Millions of American doctors, nurses, and parents got down to the serious business of vaccinating their children against polio, using a shot they’d been anticipating for seventeen years.
But the polio vaccine rollout had its challenges, including a manufacturing negligence & oversight failure that resulted in tens of thousands of polio cases in otherwise healthy children.
In May, the polio vaccination drive was temporarily suspended. Leonard Scheele, the U.S. Surgeon General, inspected the facilities of all six vaccine companies and fired the government officials he considered to be culpable; the director of the N.I.H. and the Secretary of Health voluntarily resigned. New safety procedures were developed, including an improved means of filtering the viral mix just before the formaldehyde was added. Better tests were developed to detect live virus, and stricter record-keeping was instituted. The incident could have created a vaccine-hesitancy crisis. But, incredibly, the American public readily accepted the medical establishment’s explanation for the failure, and its pledges to right the situation. The nation’s trust in medical progress and in Dr. Salk was so resolute that, when it was announced that a new, safe polio vaccine was available, parents pushed their children back to the head of the line. It’s hard to imagine such an outcome today.
The NY Times has a profile of Dr. Katalin Kariko, who struggled for decades against a system unwilling to consider and fund her ideas about how messenger RNA could be used to instruct cells inside human bodies to “make their own medicines”. Her work has culminated in two highly effective vaccines for Covid-19 and is being extended to produce possible vaccines for HIV, the flu, tuberculosis, and malaria.
Now Katalin Kariko, 66, known to colleagues as Kati, has emerged as one of the heroes of Covid-19 vaccine development. Her work, with her close collaborator, Dr. Drew Weissman of the University of Pennsylvania, laid the foundation for the stunningly successful vaccines made by Pfizer-BioNTech and Moderna.
For her entire career, Dr. Kariko has focused on messenger RNA, or mRNA — the genetic script that carries DNA instructions to each cell’s protein-making machinery. She was convinced mRNA could be used to instruct cells to make their own medicines, including vaccines.
Stat also wrote a piece about Kariko and the development of the mRNA vaccines. It seems like Kariko will be strongly considered for a Nobel Prize in Chemistry for her achievements. The Covid vaccines will save hundreds of thousands of lives alone, and if mRNA can indeed be harnessed to protect against HIV and malaria, the effect on the world will be immense. Give Kariko all the prizes and whatever she wants to be happy in life — she’s earned it and more.
Update: From Derek Thompson at The Atlantic, How mRNA Technology Could Change the World.
But mRNA’s story likely will not end with COVID-19: Its potential stretches far beyond this pandemic. This year, a team at Yale patented a similar RNA-based technology to vaccinate against malaria, perhaps the world’s most devastating disease. Because mRNA is so easy to edit, Pfizer says that it is planning to use it against seasonal flu, which mutates constantly and kills hundreds of thousands of people around the world every year. The company that partnered with Pfizer last year, BioNTech, is developing individualized therapies that would create on-demand proteins associated with specific tumors to teach the body to fight off advanced cancer. In mouse trials, synthetic-mRNA therapies have been shown to slow and reverse the effects of multiple sclerosis. “I’m fully convinced now even more than before that mRNA can be broadly transformational,” Özlem Türeci, BioNTech’s chief medical officer, told me. “In principle, everything you can do with protein can be substituted by mRNA.”
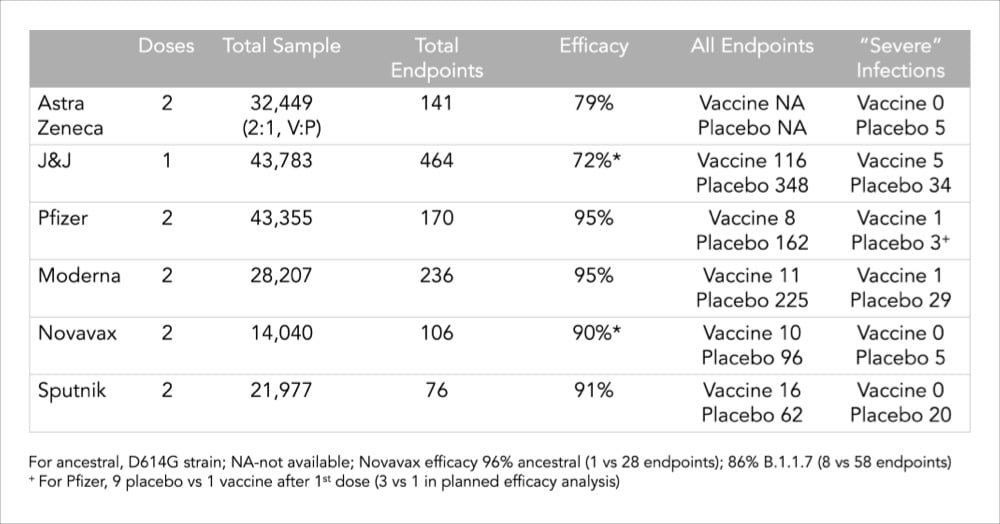
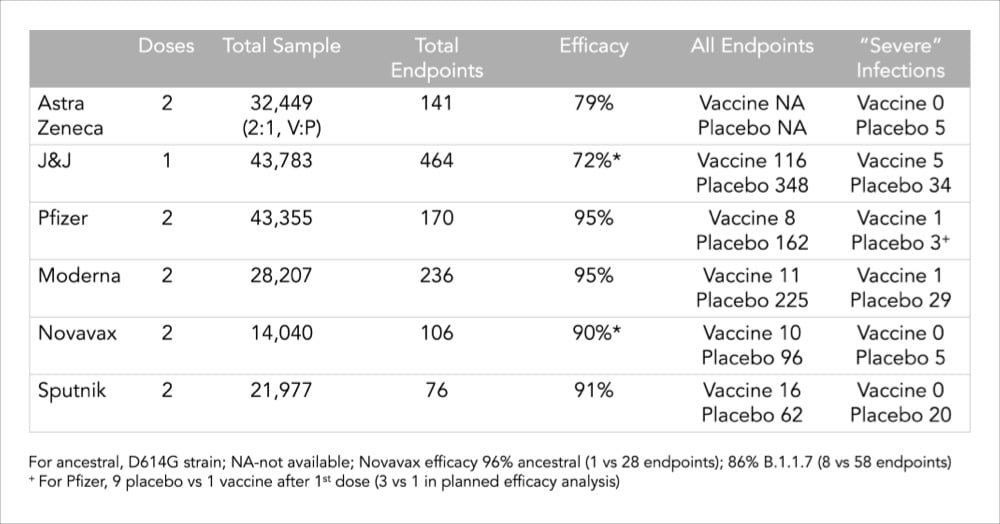
Related to my post from last month about what a 95% or 66% efficacy rate of a vaccine even means, Vox made a clear and concise video about why comparing vaccine efficacy rates is difficult — trials were done in different countries with different variants under different conditions with different levels of disease — and why protection against severe illness, hospitalization and death is a better way to compare and evaluate these vaccines. As this chart from Dr. Eric Topol shows, all of the major vaccines show strong protection against severe illness.
I thought this interview with Dr. Ashish K. Jha, dean of the Brown University School of Public Health, was really good and useful in terms of calibrating expectations with regard to the “end” of the pandemic, vaccines, and variants. On the guidance that vaccinated people should be getting:
I think it is essential that we give guidance to people. And I think we should give guidance to people on what they can do safely once they are vaccinated. People say, “Can your behavior change?” My answer is: absolutely! That’s a major motivation for getting vaccinated. First of all, what’s very clear to me is vaccinated people hanging out with other vaccinated people is pretty darn close to normal. You don’t have to wear a mask. You can share a meal. The chance that a fully vaccinated person will transmit the virus to another fully vaccinated person who then will get sick and die … I mean, sure, people get struck by lightning, too. But you don’t make policy based on that. And we need to remind people that there is a huge benefit to getting vaccinated, which is that you are safe enough to do the things you love with other vaccinated people.
According to a study conducted by the Pew Research Center, among those people who said they probably or definitely won’t get a Covid-19 vaccine, the top two reasons given were “concern about side effects” and “the vaccines were developed and tested too quickly”. For our purposes here, I’m going to ignore the first concern — the data is pretty conclusive that, on average, the vaccine side effects are minimal when compared to the effects of actually contracting Covid-19 — and focus on the quick development timeline. If you’re among those who are apprehensive about the unprecedented speed at which the world’s governments and scientific community mobilized to create several effective Covid-19 vaccines, I hope the following will help you make a good decision.
In reading a bunch of different resources (linked below throughout), I identified six main reasons why the Covid-19 vaccines were developed so quickly compared to past efforts.
1. The need was urgent. Covid-19 changed the entire world in a very short span of time and it was evident in the absence of an effective vaccine, tens of millions more people would unnecessarily die and/or suffer and the rest of us would be living in fear of disease and death. This urgency drove several of the other factors here: the availability of funding, resources, and collaboration.
2. Funding & focus. Companies and governments threw billions and billions of dollars at this. Companies, research centers, and scientists dropped other stuff they were working on to study SARS-CoV-2 and Covid-19. Governments prioritized regulatory approval for trials, etc. From a thread by Dr. Kat Arney:
Relatively few in the scientific, pharma & policy worlds care about vaccines compared w/ drugs. Most vaccine programmes are underfunded as they’re perceived as not profitable, only relevant to LMICs, & have few research groups/companies working on them. Getting funding & research capacity for vax usually takes months/years. COVID-19 vaccine was a massive global research effort w/ $millions for multiple groups/projects in weeks. Years of funding cycles & lab research happened in months, huge amount of time saved.
And from a presentation given by Dr. Anthony Fauci:
We proceeded at risk. So people say, what do you mean by “at risk”? Are you risking safety? Are you risking scientific integrity? No, it’s a financial risk. In other words, you invest in things that cost a lot of money before you even have an answer to whether the prior step worked.
And a classic example is the production of large scale amounts of clinical lots, which have been produced and are being produced before you even know that your vaccine works, so that you have hundreds of millions of doses ready to go. If the vaccine works, you’ve saved many months. If the vaccine doesn’t, you lost a lot of money, to the tune of hundreds of millions if not billions of dollars. But it was felt it was worth that investment and that risk financially in order to save time.
More on that here. As Dr. Faheem Younus put it, “We didn’t cut corners; we cut the crap!”
3. Availability of volunteers & high incidence of disease. In order to statistically show the vaccine works, you need people to test it on and you need enough people in the studies to get sick. Kat Arney again:
To show vax effectiveness, you need a high number of people with the disease in the population — big problem with the Ebola vax is that it took so long to develop the outbreak was over & the couldn’t get enough numbers to conclusively show it worked
We’re in a global pandemic — the vaccine is being tested in places with very high community prevalence, so trials can hit pre-determined statistical milestones very quickly. Huge amount of time saved.
Hundreds of thousands of people around the world volunteered to test these vaccines — without them, we’d be months and years away from a safe, tested vaccine.
4. International & corporate collaboration. Countries and companies shared research, data, and resources because the primary goal was to develop effective vaccines and save lives, not make a profit. For instance, Chinese researchers posted the genome for SARS-CoV-2 on January 11, 2020, allowing the effort to develop a vaccine to begin.
5. We knew a lot about coronaviruses from previous work. This wasn’t an effort that started from scratch. From Bloomberg:
The Pfizer-BioNTech and Moderna vaccines may seem brand new, but they are the culmination of more than a decade of work that started during the SARS and MERS outbreaks. Vaccines were even developed against MERS but were never needed. Nevertheless, scientists learned a huge amount from working with that virus, which is from the same family as the one that causes Covid-19.
From Dr. Habibul Ahsan:
Really, most of the vaccine platform development work is already done. You just have to do the remaining part, which is adding the right viral antigens to the already-proven platform and making sure it’s safe and effective in humans. Even in just the last five to 10 years, we’ve made big leaps in developing new kinds of vaccine platforms like those being tested for SARS-CoV-2.
6. Scientific and technological capability. Ok, we know a lot about coronaviruses but humanity’s general scientific and technological abilities have never been stronger or more powerful. Again from Bloomberg:
Remember also that technology has evolved rapidly — for example, we’re now about able to sequence the genomes of every mutant version of the virus in less than a day. That helps in speeding up vaccine development.
Dr. Mark Toshner sums up the effort:
However we have collectively now shown that with money no object, some clever and highly motivated people, an unlimited pool of altruistic volunteers, and sensible regulators that we can do amazing things.
Further reading: The lightning-fast quest for COVID vaccines — and what it means for other diseases (Nature), How were researchers able to develop COVID-19 vaccines so quickly? (Univ. of Chicago), The race for the COVID-19 vaccine: A story of innovation and collaboration (Carnall Farrar), COVID-19 vaccines: development, evaluation, approval and monitoring (European Medicines Agency).
Stat’s Andrew Joseph and Helen Branswell on the short-term, middle-term, and long-term future of the coronavirus in the US. The short-term outlook is dominated by vaccination & variants; some parts of the country will continue to be affected by outbreaks:
Conditions may be ripe for a better summer, however. Vaccine supplies should be flowing more freely, at least in the U.S.; the Biden administration now expects enough vaccine doses in hand for all adults by the end of May. With most vulnerable populations protected, there should be fewer hospitalizations and deaths. And with warmer weather, people can return to outdoor life.
Widespread transmission of the virus could be replaced by more sporadic and localized outbreaks. There’s also growing evidence that vaccines don’t just protect people from getting symptomatic Covid-19, but can reduce transmission.
And in the long-term, well, SARS-CoV-2 will be around for years and even decades to come:
Years from now, SARS-CoV-2 could join the ranks of OC43, 229E, NL63, and HKU1 — the four endemic, seasonal coronaviruses that cause a chunk of common colds every year. Essentially, our immune systems — primed by vaccines, boosters, and previous encounters with the coronavirus — will be ready to knock back SARS-2 when we see it again, potentially blocking an infection or leading to one that causes no symptoms or maybe just the sniffles.
It’s good to read stuff like this — it provides a basis to use when calibrating your optimism or pessimism for future activities and desires.
Zeynep Tufekci has written an important piece for The Atlantic on the mistakes that the media, public health officials, and the public keep making during the pandemic and how we can learn from them. A big one for me is how scientists & other public health officials and agencies communicate their knowledge to the public and how the media interprets and amplifies those messages.
Thus, on January 14, 2020, the WHO stated that there was “no clear evidence of human-to-human transmission.” It should have said, “There is increasing likelihood that human-to-human transmission is taking place, but we haven’t yet proven this, because we have no access to Wuhan, China.” (Cases were already popping up around the world at that point.) Acting as if there was human-to-human transmission during the early weeks of the pandemic would have been wise and preventive.
Later that spring, WHO officials stated that there was “currently no evidence that people who have recovered from COVID-19 and have antibodies are protected from a second infection,” producing many articles laden with panic and despair. Instead, it should have said: “We expect the immune system to function against this virus, and to provide some immunity for some period of time, but it is still hard to know specifics because it is so early.”
Similarly, since the vaccines were announced, too many statements have emphasized that we don’t yet know if vaccines prevent transmission. Instead, public-health authorities should have said that we have many reasons to expect, and increasing amounts of data to suggest, that vaccines will blunt infectiousness, but that we’re waiting for additional data to be more precise about it. That’s been unfortunate, because while many, many things have gone wrong during this pandemic, the vaccines are one thing that has gone very, very right.
This pair of statements she highlights — “no clear evidence of human-to-human transmission” and “There is increasing likelihood that human-to-human transmission is taking place, but we haven’t yet proven this, because we have no access to Wuhan, China” — are both factually true but the second statement is so much more helpful, useful, and far less likely to be misinterpreted by people who aren’t scientists that making the first statement is almost negligent.
A film crew from the NY Times recently spent several days in the Covid-19 ICU in Arizona, at the time one of the hardest hit places in the world. Two of the nurses wore GoPro cameras while working to witness what they did on a daily basis — the 12-hour days, the grief, the care, the constant death. This video is incredible and incredibly difficult to watch — you actually see a patient die on camera, surrounded by nurses and family (virtually).
So many Americans have died in hospitals without family by their side, but they were not alone. Nurses brush patients’ teeth, change their catheters and hold their hands in their final moments.
At the beginning of the video, one of the nurses says, “Unless you’re actually in there, you have no idea.” Thanks to their willingness to share their experiences, now we at least have some idea.
Update: Vox talked to some ICU doctors about what it’s like for their patients when they die from Covid-19. Because of patient confidentiality and the contagious nature of the disease, society (and even the families) has been “protected and sheltered from seeing the worst of this disease”.
Imagine trying to breathe through a very narrow straw, says Jess Mandel, chief of pulmonary, critical care, and sleep medicine at UC San Diego Health. “You can do that for 15 to 20 seconds, but try doing it for two hours.” Or for days or weeks.
Patients struggling through low oxygen levels like this have told Kenneth Remy, an assistant professor of critical care medicine at Washington University School of Medicine in St. Louis, that it feels like a band across their chest or that their lungs are on fire. Or like a thousand bees stinging them inside their chest. Others might have thick secretions in their lungs that make it feel like they are trying to breathe through muck. Many people say it feels like they’re being smothered.
The ordeal is so taxing that many wish for death. “You hear the patients say, ‘I just want to die because this is so excruciating,’” Remy says. “That’s what this virus does.”
In popular press and social media, there’s been a misunderstanding of what is actually meant when scientists say that the Pfizer and Moderna Covid-19 vaccines have an efficacy of 94-95%. It does not mean that 95% of vaccinated people are protected from infection — these vaccines are better than that. Dr. Piero Olliaro explains in a letter to The Lancet:
The mRNA-based Pfizer and Moderna vaccines were shown to have 94-95% efficacy in preventing symptomatic COVID-19, calculated as 100 x (1 minus the attack rate with vaccine divided by the attack rate with placebo). It means that in a population such as the one enrolled in the trials, with a cumulated COVID-19 attack rate over a period of 3 months of about 1% without a vaccine, we would expect roughly 0.05% of vaccinated people would get diseased.
Another way to put it: you’re 20 times less likely to get Covid-19 with a vaccine than without. (And again, data indicates these are safe vaccines.) Olliaro explains with some simple math:
If we vaccinated a population of 100,000 and protected 95% of them, that would leave 5000 individuals diseased over 3 months, which is almost the current overall COVID-19 case rate in the UK. Rather, a 95% vaccine efficacy means that instead of 1000 COVID-19 cases in a population of 100,000 without vaccine (from the placebo arm of the abovementioned trials, approximately 1% would be ill with COVID-19 and 99% would not) we would expect 50 cases (99.95% of the population is disease-free, at least for 3 months).
And of course if you vaccinate widely, it becomes a compounding situation because the virus just runs out of people to infect.
Over the past week or two, I’ve read a number of articles and threads about why Covid-19 cases are falling so rapidly in the US. The explanations have all been somewhat unsatisfying to me. Cases have indeed dropped off quite quickly and it happened pretty uniformly all over the country. Look at the mini state graphs on the NY Times Covid page — they all look about the same. Hospitalizations and positivity rates have dropped too, so while the number of daily tests has fallen too, this appears to be a real drop and not just an artifact of a lack of testing. Which is great news! Imagine a February and March that looked like December — a disaster compounded.
So what’s going on here? For The Atlantic, Derek Thompson lists four reasons for the decline in cases and hospitalizations that mirror the arguments I’ve seen elsewhere: “social distancing, seasonality, seroprevalence, and shots”.
The vaccine explanation is the weakest one for me: not enough people outside of healthcare workers had gotten them early enough to start bending that curve sharply downward in early January. But as Thompson notes, it could be having more of an effect on hospitalizations because the folks getting shots (and therefore immunity against severe infection) are those most likely to end up in hospitals due to infection. And obviously, vaccines are going to become the dominant factor in falling case numbers as more and more people get jabbed.
I’m also skeptical of the seasonality argument, but (again, as Thompson notes) there’s a lot we don’t know about how temperature, sunlight, humidity, and this specific coronavirus interact. Obviously Covid-19 is a seasonal thing and that’s definitely a contributing factor here, but that sharp of a drop in early January? I don’t know if it’s the primary driver here. Also, the seasonal flu typically peaks in February in the US.
The seroprevalence argument is an interesting one. Here’s Johns Hopkins infectious disease epidemiologist David Dowdy in a great Twitter thread about the US case decline:
I think the most logical explanation is one proposed initially by @mgmgomes1 and others — namely that we are seeing the effects of population immunity with heterogeneous mixing + strong behavioral effects. Take a(n overly) simple example. Assume 60% of a population has zero respiratory contacts, while the other 40% lives life as normal. If 75% of that high-mixing group has immunity (e.g., 30% population seroprevalence), you could easily see herd effects.
Basically, a large percentage of the folks at the greatest risk of getting Covid-19 in the US (i.e. folks who aren’t able or willing to keep from seeing other people and/or take proper precautions) have gotten it, resulting in a sort of localized “herd immunity” among those folks. After the massive holiday surge in cases (more on that in a sec), this hypothesis suggests, the virus started running out of people to infect and rates dropped quickly. This is the first explanation I read that really made sense to me.
Thompson leads off his piece with the behavioral explanation: “Maybe Americans finally got the hang of this mask and social-distancing thing.” I do not buy that people who previously weren’t doing so before suddenly started wearing masks (or better masks), keeping distant, spending less time indoors with others, and staying home from work started doing so in numbers large enough to cause such a sharp downturn. But you can’t consider the decline without also looking at how cases got so high in the first place. Here’s Steven Johnson on Twitter, zooming out a few months:
[It’s] not so much that people got the hang of social distancing, but rather that the holiday season compelled people to relax social distancing for in-person family gatherings. So the current decline is mostly reversion to where we were in Oct-Nov.
Yes, this. Without these holidays, we may have seen much more of a winter plateau than a spike. So here’s what seems plausible to me. As the cold weather made the coronavirus more effective at infection, people gathered for Halloween, Thanksgiving, Hanukkah, Christmas, and New Year’s — each subsequent holiday building on the previous one — and it pushed cases much higher than they would have been without those major gatherings. After two months of massive infection rates, the virus burned itself out among the high-mixing group and everyone else retreated back into their homes and pods to hunker down, resulting in the steep decline we’re seeing.
Obviously, careful scientific study will be necessary to tease out how significant each of these (and other!) causes were to the holiday spike and subsequent decline. But for now, the way forward is continuing to social distance, wear (better) masks, limit close contacts, and get people vaccinated — before B.1.1.7 and the other variants hit.
So, I got a link to this video from a reader and didn’t know anything about it going in, aside from the title (“Chris Finds Out If He Has HIV”) and the reader’s comment (“American health care system”). Here’s the deal — radiologist Dr. Chris Nicholas was accidentally exposed to HIV at work and this video documents a twin journey: 1) he learns way more about HIV/AIDS than he did in medical school while trying to understand what the exposure means for his health, and b) the absolutely maddening battle that he, an actual doctor and very knowledgable & capable patient, has with the absurd “system” of American health care that works to bury people in circuitous phone calls, gotta-be-perfect paperwork, and pass-the-buck bureaucracy to avoid providing necessary medical care. The phone call with the pharmacist at the 27:05 mark would be the height of absurdist humor if it weren’t so infuriating.
If an actual health care professional had to work this hard to get what he needed, what are the chances that someone without his level of knowledge, time, and resources is going to be able to? This whole extractive, regressive system needs to fucking go. (thx, matt)
Newer posts
Older posts







Socials & More